Cancer journey extends UMMC professor’s lessons beyond classroom
Dr. Stanley Smith first saw the University of Mississippi Medical Center through the care that added years to the lives of his grandmother, mother and father. As a patient of the UMMC Cancer Center and Research Institute, he’s now experienced that same compassionate medical treatment firsthand.
“I’ve always been on team UMMC,” said Smith, professor of advanced biomedical education and pharmacology/toxicology at the UMMC School of Medicine. “I trust people here, and as a UMMC patient, you can talk to the right ears and benefit from the tremendous depth of expertise.”
That skill, combined with compassion, Smith said, was his first introduction to UMMC. Smith’s mother, Catherine Smith of Longview, near Starkville, was treated at UMMC for cervical cancer in 1993, living another 16 years after diagnosis.
His grandmother, Sue Willie Bell, had developed an infection on her foot in 1968, the result of type 1 diabetes. When the infection spread to her leg, she was turned away from her local hospital and sent home to die. Her employer took her to UMMC, where her leg was amputated to save her life. She lived another five years. In 2013, Smith’s father, Archie Smith, presented with a very complicated illness that was slowly killing him. Physicians at UMMC, in particular, the geriatrics group, solved the riddle and saved his life. Their valiant efforts allowed him to live long enough to meet Smith’s wife, Anne.
“And now I have benefited from that level of care,” he said.
Smith had been keeping track of his PSA, an acronym for prostate-specific antigen, a protein that’s produced by normal and cancerous cells of the prostate gland. A PSA blood test is used to screen for prostate cancer.
A PSA level of 4 or above can result in a recommendation for a prostate biopsy, and Smith’s kept creeping higher. Blood in his urine brought him to Dr. Charles Pound, chief of the Division of Urology, but that symptom went away. An enhanced PSA test that includes several biomarkers followed, registering a level just about 10. A prostate biopsy showed that Smith was in the early stages of prostate cancer; a PET scan showed the cancer hadn’t spread.
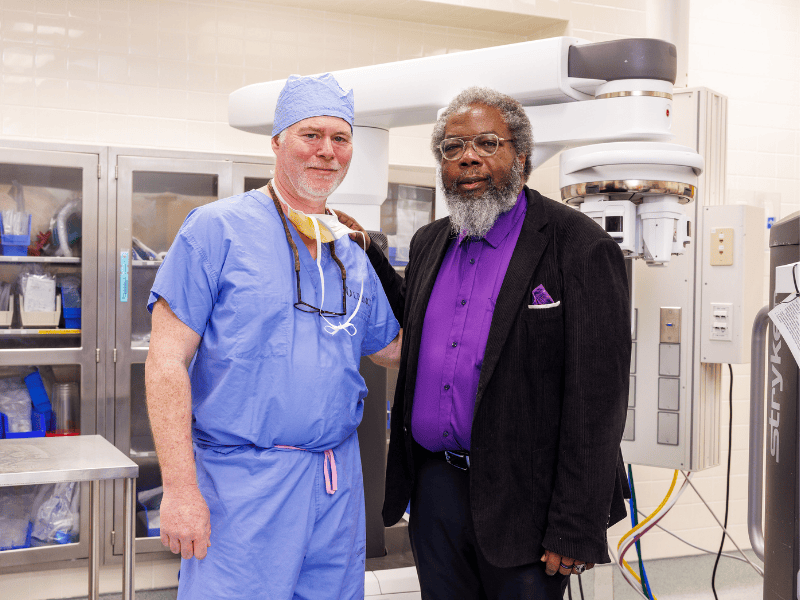
“Dr. Smith did exactly what we encourage all men to do—pay attention to changes in their PSA and seek care early,” said Dr. Charles Pound, chief of the Division of Urology. “Because his cancer was detected at an early stage, he had multiple effective treatment options and an excellent prognosis.”
Smith had several options – surveillance, hormonal treatment or removing the prostate. “Given my age and the risk, I chose surgical treatment,” he said.
Prostate cancer is the most common cancer and the second leading cause of cancer death among men in the United States. Detecting prostate cancer early through PSA tests can help men live longer.
African American men, who have a greater chance of developing prostate cancer, and men with a family history of prostate or other cancers, should discuss PSA screenings at 40. Otherwise, screening is recommended for men 45 and older.
Smith, who arrived at UMMC in 1987 as a graduate research assistant, is best known for his talents as a teacher, having trained decades of medical school graduates in pharmacology and toxicology. His teaching didn’t stop when he became a patient.
“We’re a teaching hospital, so I saw several M3s and residents who I recognized during my treatment,” he said. “They were all very professional and made me proud. I told them if I could teach them in the classroom, I trust them and their training and would gladly help teach them as a patient in the surgical suite.”
Smith opted for daVinci robotic surgery, which had the advantages of being less invasive.
“Robotic prostate surgery allows us to treat cancer effectively while minimizing discomfort and recovery time,” said Dr. Chad Huckabay, associate professor of urology and Smith’s surgeon. “Dr. Smith was an excellent candidate, and his commitment to following his recovery plan helped him return to normal life quickly.”
Smith underwent surgery Oct. 28. “My recovery took about three weeks,” he said. “By Thanksgiving, I noticed that I was feeling like myself again.”
His support of CCRI and its journey toward NCI designation was strengthened following his experiences as a CCRI patient, Smith said.
“I believe we will reach that goal,” he said, “because we have plans in place that will move us forward with purpose and ensure we meet every requirement for NCI designation.”
Mississippi continues to face some of the nation’s highest cancer incidence and mortality rates. Strengthening the state’s cancer infrastructure through the CCRI’s journey toward NCI designation is aimed at changing that, Smith said, citing his cancer care as a sign of what’s possible when patients have access to comprehensive, world-class cancer services.
“If there is one thing I have taken away from CCRI care at UMMC, it is this: Trust in my health care providers,” Smith said. “Because of that, I didn’t worry or have fear or trepidation and could focus on getting better.”


