UMMC first in state to offer CAR T therapy for persistent cancer
When Patricia Hurrod's aggressive cancer continued to defy chemotherapy and radiation, she found hope in a groundbreaking, advanced treatment offered only in the state at the University of Mississippi Medical Center.
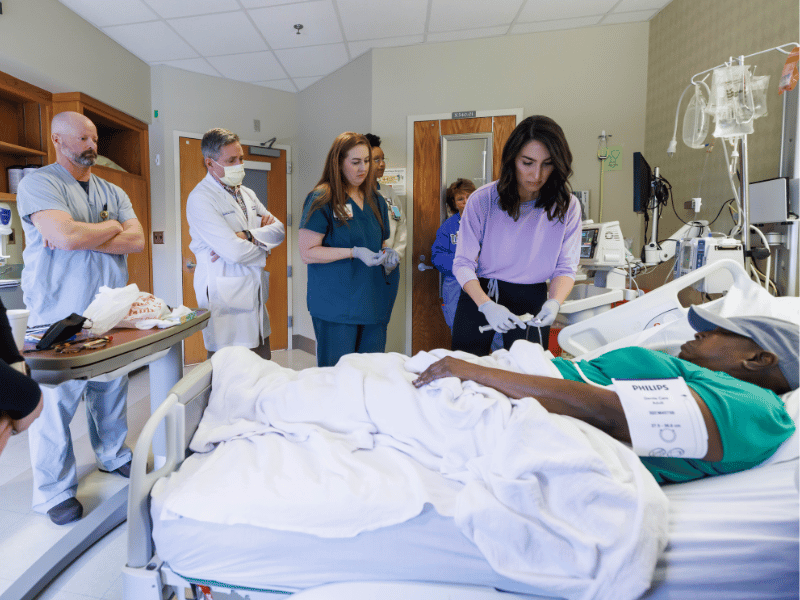
The UMMC Bone Marrow Transplant Unit recently introduced a new treatment for patients with cancer. Chimeric antigen receptor T cell, or CAR T, therapy is a cancer treatment altering the patient’s own T cells (immune cells found in bone marrow) to better recognize and destroy cancer cells.
Hurrod, a native of Clinton, explained that she had been in and out of the emergency room for months, complaining of throat pain, but physicians couldn’t detect anything out of the ordinary. When an ear, nose, throat specialist finally removed her tonsils, the organs tested positive for B cell lymphoma.

After six rounds of chemotherapy, Hurrod said the cancer had all but disappeared. But three months later, the aggressive lymphoma had returned. She was then referred to Dr. Vincent Herrin, UMMC professor and director of the hematologic malignancies program, for BiTE therapy, an immunotherapy therapy shown to have better results than chemo and radiation therapy.
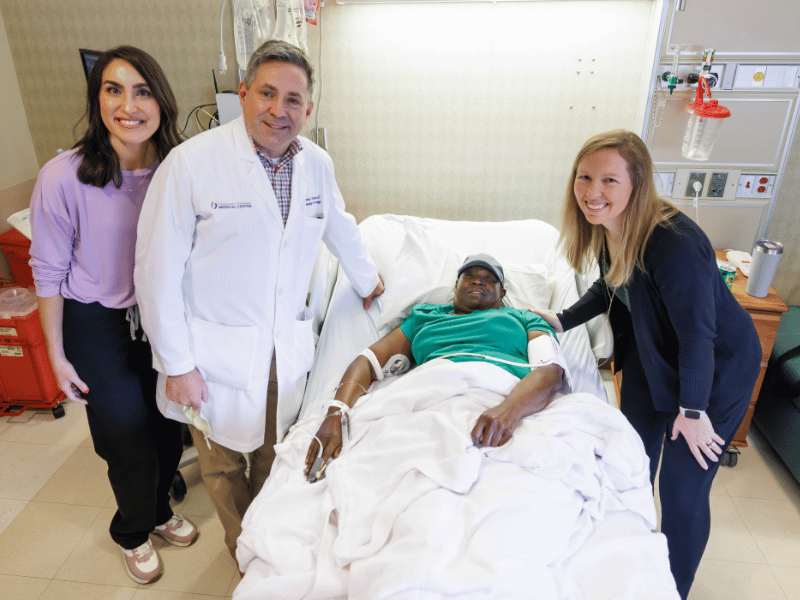
“When we saw how aggressive her cancer was, I knew she needed something stronger,” Herrin said. “B cell lymphoma is often cured with chemotherapy, but hers was not reacting well to it. A patient like her is an ideal candidate for CAR T therapy. Having this program in place was a way to offer her life saving treatment.”
“Our bodies don’t fight off cancer because they don’t recognize it as something foreign,” said Pam Farris, former nurse manager of BMT and an integral figure in the acquisition of this technology at UMMC. “So, what CAR T does is essentially attach a homing beacon to the T cell that homes in on that specific cancer cell and kills it immediately. Your own body starts killing cancer.”
Because the tumor was growing rapidly, Hurrod had to undergo chemotherapy almost daily for several months until CAR T could be administered. She said she was so sick by that time that she was ready to try anything.
“Being the first person to have the treatment here, I was just praying that this was the right procedure for me,” she said. “I remember that day—when they put the cells back in—but I don't remember going back to Hope House, going back and forth to the hospital, or any of that.”
CAR T therapy is known to cause two major side effects: cytokine release syndrome and encephalopathy. Cytokine release syndrome occurs when large amounts of white blood cells—T cells in this case—are activated and release inflammatory cytokines, a signaling molecule that promotes inflammation. In immunotherapy patients, encephalopathy or changes in the way the brain functions, is caused by the discarded “cell trash” entering the bloodstream. This can cause confusion, agitation, memory loss, depression and exhaustion.
Following the treatment on February 16, Hurrod lost about a month of time before she felt like herself again.
“I was semi-conscious but wasn’t conscious enough to know what was going on,” said Hurrod. “When I really woke up and could notice things, I told my daughter that the clock was wrong. She said ‘Mama, the time changed. It’s March now.’”
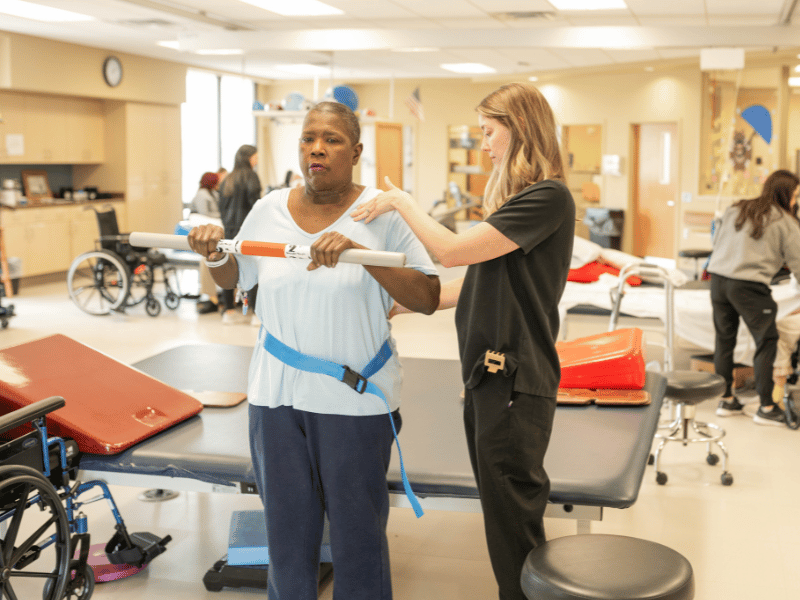
Soon after, Hurrod was referred to Methodist Rehabilitation Center, where she received physical and occupational therapy to regain her strength and mobility.
Lindsey Klaus, the occupational therapist who was responsible for Hurrod’s care at MRC said she worked hard and was able to go home after about 10 days. “She was a great patient,” said Klaus. “She was always eager to come to therapy. She came to us needing about 50% help with all her daily activities and left not needing any kind of physical assistance.”
Following her 100+ day post-treatment scans on May 15, Hurrod’s physicians said she looks like she could make a full recovery. With this technology available at UMMC, she and other patients across the state now have a chance to move forward with their lives.
“With CAR T, we are able to save lives we wouldn't have otherwise been able to, so it’s an exciting thing to be a part of,” said Dr. Carter Milner, professor of hematology and oncology and bone marrow transplant. “The patient has a small amount of activity in that area on the PET scan that we expect to continue to improve. She isn’t in complete remission yet, but she’s had a great response to the treatment that we hope will continue.”
“Due to the expertise of our Bone Marrow Transplant Team at UMMC and the leadership of Dr. Milner, we are extremely excited to be the only institution in the state to offer this highly effective cell-based therapy of CAR-T,” said Dr. Rodney Rocconi, director of the UMMC Cancer Center and Research Institute and Ergon Chair of Cancer Research. “The ability of reprograming a patient’s own immune system to attack their cancer cells is a tremendous advancement in cancer therapy, and our patients deserve the access to these types of treatments to improve their survival.”


