Novel treatment could protect, rescue damaged kidneys
It’s been decades since a new pharmaceutical for kidney disease has crossed the threshold into patient care. Now, a team of scientists have put their foot in the door.
A study published in the journal Science shows that a new experimental drug rescues damaged kidney cells in two animal models of renal disease. Harvard Medical School scientists led the international team, including University of Mississippi Medical Center researchers, in making the discovery.

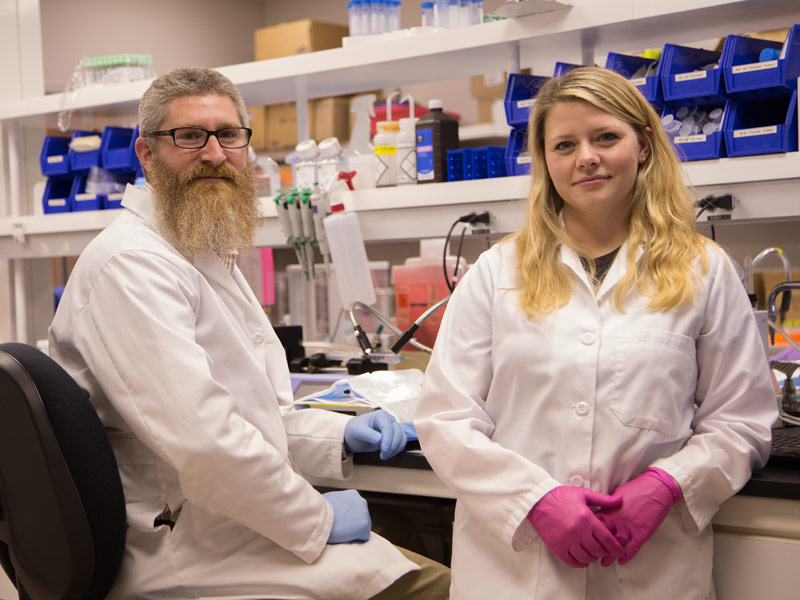
Dr. Anna Greka, a physician-scientist at Harvard Medical School and Brigham and Women’s Hospital, led the study. Her lab enlisted the help of Dr. Michael Garrett, UMMC professor of pharmacology and toxicology, to conduct a key confirmatory experiment.
“This study is a great example of collaborative science,” Garrett said. “We were able to fulfill a need.”
And for patients with renal disease, there’s a substantial need.
“For the past forty to fifty years, there have been no drug discoveries for progressive, chronic kidney diseases,” Greka said. These diseases affect hundreds of millions of people worldwide, contributing to the deaths of more than 40,000 Americans each year.
For this particular study, her lab used a transgenic rat model that develops a rare, genetic form of kidney disease. A molecular chain reaction that occurs in this model creates a “vicious cycle,” Greka said, which leads to the destruction of specialized cells called podocytes. Foot-like extensions stemming from these cells surround small blood vessels and help filter blood through the kidneys. Prolonged damage to podocytes may lead to chronic kidney disease or renal failure, and their loss is irreversible.
“If the podocytes die, they are gone forever,” Greka said.
Their lab found that an experimental drug, called AC1903, targets the cycle by inhibiting a particular protein, breaking the chain reaction. After treatment, rats with progressive kidney damage had a higher number of podocytes and decreased amounts of protein in their urine, a marker of recovered kidney function.
However, Greka needed to know if the treatment worked in another more common model of kidney disease. That’s when she contacted UMMC’s Garrett, who studies the genetics of hypertension and kidney disease.
“Two-thirds of people with chronic kidney disease also have hypertension or diabetes,” Garrett said. “Most of the current pharmacological approaches to treating renal disease focus on these underlying causes, but no drugs work directly on protecting or restoring kidney cells.”
The Garrett lab tested AC1903 in Dahl salt-sensitive rats, which develop high blood pressure and severe kidney damage when fed a high-sodium diet.
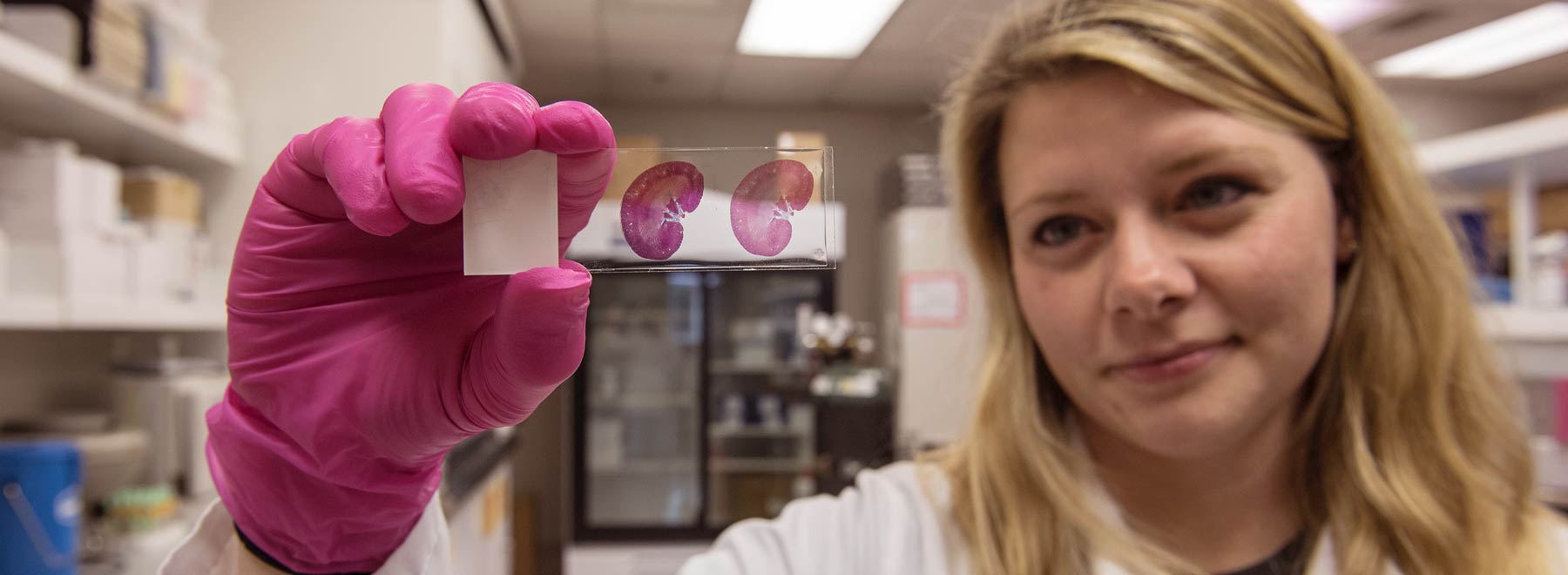
“The Harvard scientists were interested in using this model,” said Ashley Johnson, a scientist in Garrett’s lab. She conducted a series of experiments designed to learn if the compound had similar effects on kidney damage resulting from hypertension.
After treatment, Johnson and Garrett observed decreased proteinuria and increased podocyte numbers, consistent with the results found at Harvard.
“It’s encouraging to find the answer you expected,” Johnson said.
Both of these models show signs of focal segmental glomerulosclerosis, a form of scarring that is a leading cause of kidney failure in humans. Even though the damage has different causes – one inherited, one acquired through other diseases – AC1903 appears to work in both cases. This is important because many instances of renal disease have multiple causes.
“Genetics can increase a person’s susceptibility to kidney damage, but other conditions like hypertension and diabetes can exacerbate the risk,” Garrett said.
“If this potential therapeutic becomes a treatment, combining it with another medication like an anti-hypertensive drug could be an effective approach to treating forms of kidney disease,” he said.
Both Garrett and Greka expressed positive experience with their collaboration, keeping open possibilities for future work together.
In regards to AC1903, there’s still plenty of work to do, even after several years of study. The next steps, Greka said, are to conduct further pre-clinical testing to gauge toxicity and to create more effective, drug-like versions. Eventually, she hopes to see it in human clinical trials. However, the finding is already a huge step forward in a field with limited recent progress.
“We are able to show that this small molecule can treat kidney disease from multiple causes,” Greka said. “This is transformational work.”
Investigators from the Gachon University in South Korea, Heidelberg University in Germany, Charles A. Drew University in California and the University of Nebraska Medical Center also contributed to the research.