New process shortens time to breast reconstruction
Making recovery easier and quicker for patients is the goal of a new procedure the University of Mississippi Medical Center’s Cancer Institute is offering women seeking breast reconstruction after a mastectomy.
“I wanted to eliminate as many steps as possible,” said Maria Ricketts of Madison, a breast cancer survivor who is among the first to use the new expanders.
Traditionally, doctors who work with breast cancer patients remove the malignant tissue and for those who want reconstruction, begin the process of stretching the skin to insert implants. They can insert a tissue expander at the time of the mastectomy, said Dr. Ben McIntyre, an associate professor of plastic surgery and member of the Cancer Institute’s Interdisciplinary Breast Cancer team.
“Once a week we’d access the expander, basically a water balloon, with a needle and add saline,” he said. Patients had to return to the doctor for each injection.
This new type of tissue expander uses air to help stretch the skin and the patient can operate it from home.
“It’s got a remote, and the patient can do it at home now,” McIntyre said. “I see patients who are three hours away. This is much better for them.”
The final step is to remove the expander and surgically insert more permanent saline or silicone implants. Air expanders lessen the time to that surgery.
“The air expander goes quickly,” McIntyre said. “Rather than several months with slow additions of saline once a week, they may be ready for their final surgery in four to six weeks.”
McIntyre said the air expanders have several advantages, including:
- Since there are no needle pricks, there’s less chance of infection.
- Patients can operate the expanders from home, sometimes up to three times a day.
- Patients have fewer clinic visits.
Ricketts, who now looks forward to returning to work, said, “I think it’s cool that I got to experience something new. It’s a bit painful because you are doing something to your body that nature doesn’t do, but it’s good because it’s simple.”

Ricketts, who teaches Spanish and French at Jackson State University, discovered her cancer with a routine mammogram. “I came back for a 3D and everything just came down on me.”
With an attitude of “whatever you can learn, it’s never too much” she began researching her cancer.
“It hit me the first time I saw an oncologist,” she said
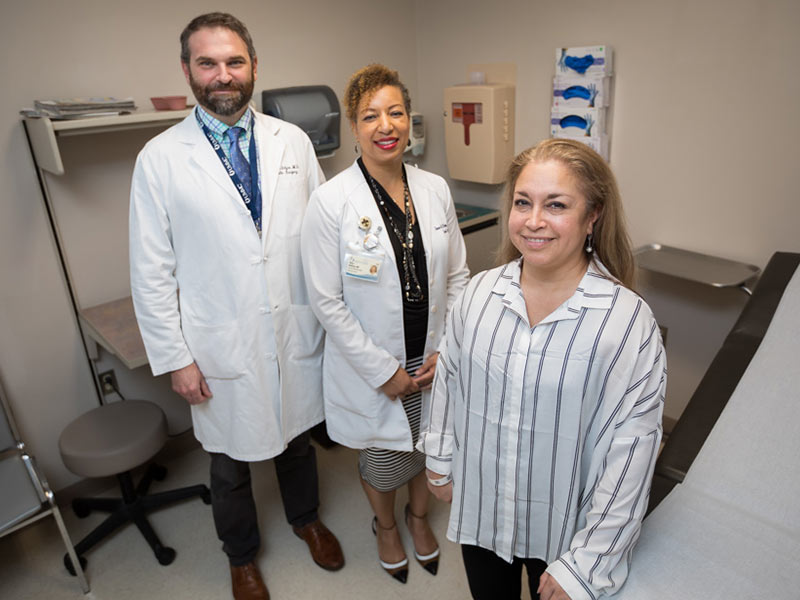
Her medical oncologist, Dr. Natale Sheehan, assistant professor of medicine, said because Ricketts was diligent about getting her mammogram and because her cancer, ductal carcinoma in situ, was caught so early, she had a choice of appropriate treatment options.

“She chose bilateral mastectomy instead of a mastectomy and taking chemoprevention therapy,” Sheehan said. “The chemoprevention decreases the risk of developing another area of cancer in any remaining breast tissue.”
“I chose the most radical approach,” Ricketts said of her decision to have both breasts removed. “I never want to have to go through this again.”
During Ricketts initial surgery, Dr. Shawn McKinney, associate professor of surgery, did the mastectomies and McIntyre started the reconstruction process.
McIntyre said Ricketts was a good candidate for this type of reconstruction.
“We try to match those who are a good fit and have an interest in it,” he said. “I foresee more and more people coming in and requesting to have the air expanders.”
Each patient’s case is fully discussed with members of the Interdisciplinary Team. For example, if a patient needs radiation therapy, doctors consult on when and how to deliver it before therapy starts.
Until recently, McIntyre said, the procedure had not changed in 40 years. “It’s been a salt water balloon we pump up.”
The new process has some drawbacks: “They only make three sizes,” he said. “This won’t fit some patients based on their skeletal framework.”
Coaching precedes use. Patients are taught how to inflate the expander, what signs to look for in using it and when to contact their medical providers.
Occasionally, patients are advised to slow or stop the process for a time then start again.

Ricketts calls her cancer journey one filled with fear, self-reappraisal and joy.
Time in her backyard with her dogs, Boo Boo and Pug, and gardening brought serenity; care provided by her husband and daughter brought joy; and continuing to teach online classes helped her maintain normalcy.
Soon she’ll return to the JSU classroom, teaching elementary Spanish. Her recovery continues and has reached the point she’s annoyed when she realizes she can’t yet pick up some objects.
Her daughter, Alexa, 17, continues to help. “She has been my rock,” Ricketts said. Her son, Javier Rodriguez, 29, keeps tabs from out of state.
She’ll continue to see the UMMC Interdisciplinary Breast Care Team. “It’s amazing how well they coordinate. I was advised of all the steps. Their intent is to get the person well.”


