Gamma Knife offers noninvasive care for brain tumors
New radiosurgery equipment at the University of Mississippi Medical Center means new hope for many Mississippians with brain tumors or brain metastases.
For many, like Neeru Sharma of McComb, the treatment can be completed in one day.
The Department of Radiation Oncology operates the Gamma Knife at the UMMC Cancer Institute at the Jackson Medical Mall Thad Cochran Center.
Sharma was referred by her physician in McComb after he found her breast cancer had metastasized to her brain.
While she doesn’t call the experience pleasant, Sharma said, “When you trust your doctors it makes it easier.”
Fitted with a mesh mask, Sharma's head was immobilized while doctors used radiation to attack two small tumors in her brain. “It was hard,” she said. For about 50 minutes she lay “with my eyes closed, staying still and the pressure on my forehead.”
It was uncomfortable, but understanding the process before therapy helped, she said. Doctors and staff explained what would happen in detail, including the pressure on her forehead designed to keep her head still.
“You did very well and you didn’t move at all,” Dr. Roberto Rey-Dios, assistant professor of neurosurgery and a member of the team that administers treatment, told her.

“The Gamma Knife is tried and true,” he said. “We have an updated version that has capabilities not previously available at UMMC.”
Rey-Dios said Gamma Knife technology has been in use for more than 30 years and physicians have developed proven standards for using it.
“It has an extremely high accuracy because it has no moving parts," he said. "Other machines have moving parts, so accuracy may not be the same.” Rey-Dios has performed more than 200 Gamma Knife surgeries.
For those with cancers that have metastasized to the brain, Gamma Knife surgery is “potentially curative,” Rey-Dios said.

Dr. John Ruckdeschel, UMMC Cancer Institute director, called the Gamma Knife "one more addition to our armamentarium against brain tumors."
"It allows us to more focally attack a site of cancer without having to give radiation to the whole brain, which can often result in side effects of its own," Ruckdeschel said. "It is one more example of care that is only available at UMMC’s Cancer Institute.”
Its pinpoint accuracy enables providers to target lesions, giving patients better cognition after therapy, said Dr. Srinivasan Vijayakumar, chair of the Department of Radiation Oncology. The machine has two unique characteristics, he said.
First, it comes with a CT scanner so providers can do a scan immediately before treatment.
“We can confirm the accuracy of treatment right before we treat it," he said. "This doesn’t exist in earlier machines.”
And second, depending on the therapy needed, doctors often can use a mask instead of a metal frame that has to be screwed into a person’s head.
A mask is a mesh-like mold of the person’s head that fits over the face and head during treatment. The team also is capable of administering anesthesia for those who are claustrophobic or for children.
This type of radiosurgery produces results with less harm to normal tissue, Vijayakumar said. Cancer providers can highlight areas as small as 1 mm.
By choosing which “holes” or collimators in the dome of the machine to use, providers can deliver maximum radiation to a tumor while generating much smaller doses to healthy tissue.
The procedure may be recommended for patients with:
- Benign or malignant brain tumors,
- Metastasis of other cancers to the brain,
- Certain blood vessel disorders of the brain,
- Some types of cancer of the eye,
- Epilepsy caused by a brain tumor, or
- Trigeminal neuralgia, a nerve disorder that causes facial pain.
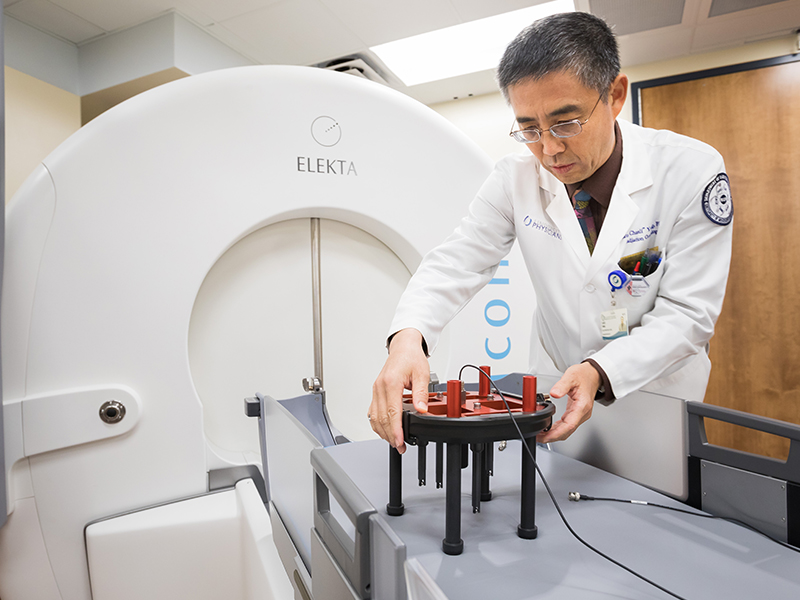
The Elektra Icon Gamma Knife offers an alternative to surgery or whole brain radiation for metastatic disease.
“Whole brain radiation for metastatic diseases leads to poor quality of life,” Vijayakumar said. “Here, we can treat only the lesions and give them better cognition in later years of life.”
Many of the more than 35 patients who have received Gamma Knife treatment since it went live in May were treated for metastatic disease, he said. Treatment can improve their quality of life and in some cases, help alleviate pain.
That’s what it did for Sharma, who began having headaches in June before receiving treatment in July. The goal is to provide curative care for her, but that must be confirmed in the coming months with periodic MRIs.
Since the Gamma Knife often can accomplish its goal with one treatment, it’s easier on the patient, said Dr. Madhava Kanakamedala, assistant professor of radiation oncology and the radiation oncologist on the team.
“For brain mets we often can do a single treatment,” he said. “For larger tumors, we can do fractionated treatments” that may take four or five days. Traditional whole brain radiation can require a patient to be in treatment five days a week for four weeks or longer.
When the $4.5 million Gamma Knife was installed, it came with the latest technologic upgrades available, a stipulation of the purchase agreement.
Upgrades include the attached CT scanner that enables physicians to verify the position of the tumor after the patient is ready for treatment and an infrared camera that detects motion and warns the team, helping to more accurately deliver therapy.

Patients treated at UMMC are evaluated by the UMMC Cancer Institute’s Interdisciplinary Brain and Central Nervous System Care Team before treatment. This enables neurologists, neurosurgeons, radiation oncologists, medical oncologists, radiologists, pathologists and others to meet and discuss what treatment is needed, the order in which it should be given and care that may be needed after treatment.
“We’ve started reviewing all brain met patients in this conference,” said Dr. Mark Anderson, assistant professor of neurology and a neuro-oncologist who co-chairs the brain care team with Rey-Dios. Anderson said the Gamma Knife is a powerful tool that can provide a better quality of life than other therapies.
Reviewing patients as a team improves each patient’s access to therapy and improves the continuity of care, Anderson said. The same team that initially reviews treatment recommendations will monitor the patient throughout therapy.
If the Gamma Knife doesn’t work, patients still have the option of using whole brain radiation later, Anderson said.
A new MRI, installed by the UMMC Department of Radiology, also aids in therapy planning, Anderson said.
Kanakamedala said after a treatment course is determined, a smaller team that includes radiation oncologists, neurosurgeons, physicists and others meets to examine treatment dosages, delivery and timing.

