Rarely used procedure promising tool for patients with abdominal cancer

Darrell Freeman is in the middle of building a storage shed and has his eye on constructing an electric motorcycle.
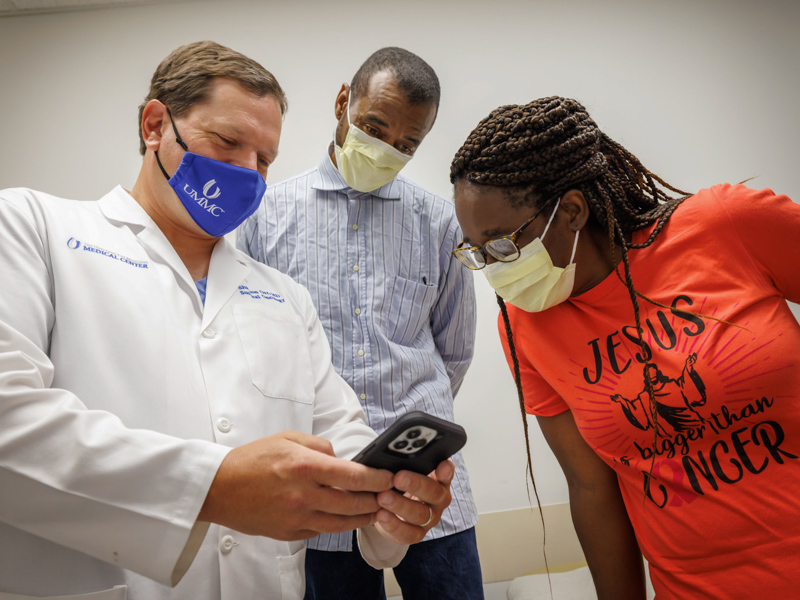
Cancer put the Hattiesburg resident’s do-it-yourself projects on hold, but a rare procedure performed by a University of Mississippi Medical Center surgeon has Freeman’s cancer on the run and life back on track.
“I’m doing pretty good,” Freeman, a computer technician at the Stennis Space Center in Hancock County, said following his April surgery for an abdominal cancer that started out in his appendix and colon, impacting the lining of those organs.

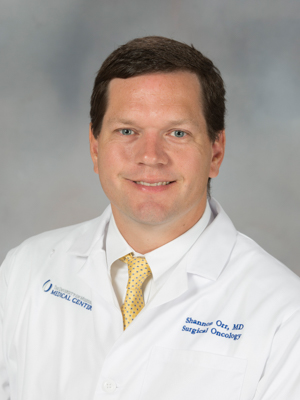
Dr. Shannon Orr, associate professor of surgery, performed the extremely uncommon HIPEC, or hyperthermic intraperitoneal chemotherapy. It’s used for removal of abdominal tumors and mucin secretions, and any other malignant tissues.
But what’s different about HIPEC is just how that cancer is removed. During the complex surgery that can take as long as seven or eight hours, the surgeon floods the patient’s abdominal cavity with a heated saline and chemotherapy solution to destroy microscopic cancer cells.
The procedure usually calls for a large incision to access the abdomen – but Orr performed it robotically, making a rarely performed procedure even more unique and elite.
The Medical Center is the only hospital in Mississippi, and one of very few in the region, that has the expert staff needed to perform the HIPEC.
“You have to have the right patient, and the right disease, to make sure you have a good outcome that will benefit the patient,” Orr said. “We remove all of the visible disease.”
And because the patient is in surgery for so long, he or she must be healthy enough otherwise to withstand the rigors, including prolonged anesthesia.
Unlike chemotherapy outside of surgery, chemo administered during HIPEC is much more potent and a much higher dose. “Blood flow to cancers in the lining of the peritoneal cavity or to the underside of the abdomen isn’t as good as to the liver or lungs, so chemo given systemically isn’t as good,” Orr said.
In addition, chemo administered during surgery is heated. “That’s more toxic to cancer cells,” Orr said.
Freeman’s cancer of the appendix was discovered almost three years ago by a provider on the Gulf Coast. When his appendix was removed, the surgeon found there was also cancer in his colon and abdominal wall. Freeman additionally suffered from mucinous fluid, a jelly-like material in his abdomen formed by tumors.
His provider referred him to Orr for further treatment. Orr, who performed the Medical Center’s first HIPEC surgery in 2016 on a patient who today is disease-free, saw Freeman as a good candidate for the procedure to be done robotically.

Freeman’s cancer “was caught very early. His pathology was favorable, and his CT scans looked very good.
“In most people I see, their tumors have ruptured, or they have a lot of disease. You can’t see all that robotically and clear the disease,” Orr said.
Before the surgery, Orr took a closer look through a laparoscopic procedure in which a tiny camera captured pictures inside Freeman’s abdomen. “I made sure there was very little disease and that I could safely get his disease out,” Orr said.
During the HIPEC, Orr and his team made small, minimally invasive incisions instead of a single large incision to approach the cancer. Orr removed Freeman’s gall bladder and part of his colon and attacked the cancer in his abdominal wall by flushing it with the chemo solution.
With any robotic surgery, the patient generally has a faster recovery, less pain and a shorter stay in the hospital than with traditional surgery. HIPEC patients generally stay in the hospital a week to 10 days, and “a lot of that is recovering from the surgery itself and the bigger incision,” Orr said.
“But Mr. Freeman was in the hospital only two or three days. He also could get up and move around more quickly.”
“This has been a real trial, but I have to say the robotic surgery was a blessing,” Freeman said. “I wasn’t in as much pain as I could have been from the traditional method of being cut, and the healing process is about the same.”

A robotic HIPEC “is super exciting,” said Dr. Mildred Ridgway, associate professor of obstetrics and gynecology, who cares for patients with gynecological cancers. “As difficult as it is to come back from surgeries, this could be a game-changer.”
Four or five of her patients have had their ovarian or uterine cancers treated through HIPEC. “These are patients who had a recurrence of their cancer, or who responded well initially with other therapies. It’s a second or third attempt to try to control their disease,” said Ridgway, who assists Orr in HIPEC surgeries.
“It’s not the standard of care for this disease, but we are extrapolating what has been successful with colon cancer, and patients generally have an excellent response,” she said. “If it’s someone you think can tolerate the recovery, then we have great expectations long term.”
Orr has performed about 50 HIPEC procedures at the Medical Center. “The success rate depends on the type of cancer. Most of the time for cancer of the appendix, we’re going for a cure,” he said. For some other cancers, “we want to see long-term survival of five or six years disease-free.”
The availability of HIPEC at UMMC “is huge,” said Orr, who trained to do the procedure while completing his fellowship at MD Anderson Cancer Center. “Many patients will be in the hospital a week to 10 days. To be close to home instead of uprooting is easier for the family, economically and socially.
“As we move forward, the next big step is: Will we do this for other disease sites? This can play a role in other cancers.”
“The biggest thing is that we are the only place in the state doing this,” Ridgway said. “We’ve had exceptional outcomes. It’s definitely a developing field that will grow and be more available as time goes on.”


