Plagued by memories: UMMC leaders reflect on COVID’s 5th anniversary

Five years ago this spring, we began living or dying with COVID.
In the attempt to slow down the disease, we became bogged down in months and months of disillusionment and dissolution.
Behind our masks, we peered into other half-gone faces. We “sheltered in place,” or, at best, stood six feet apart. We were cut off from hope and each other, unable to breathe the same air together without worrying that we were getting sick together.
Among those entrusted with restoring our hope, with navigating a medical/cultural/political disaster, were leaders at the University of Mississippi Medical Center.
They included three with an emergency medicine background, people trained to work as a part of a team making life-and-death judgments quickly: Dr. LouAnn Woodward, vice chancellor for health affairs, dean of the School of Medicine and COVID incident commander; Dr. Alan Jones, currently the associate vice chancellor for health affairs and former assistant vice chancellor for clinical affairs and the COVID-19 clinical response leader; and Dr. Jonathan Wilson, chief administrative officer and COVID incident manager.
Working with them was Dr. Thomas Dobbs, now dean of the School of Population Health, who led the Mississippi State Department of Health and the statewide COVID response as state health officer.

Witnessing the wrack and ruin of COVID on patients, their patients’ loved ones and the health care workers whose emotions sometimes ran rampant like the disease they were trying to contain was Dr. Andy Wilhelm, professor of medicine and chief of the Division of Pulmonary and Critical Care Medicine who was medical director of the ICU at the time.
Like their counterparts elsewhere, these five had to make sweeping decisions about coping with an elusive and deadly force, even while fighting off their own feelings of worry, sorrow and anger during a period defined by a phrase Woodward said she grew to hate: “these unprecedented times.”
Here are their recollections.
[In early December 2019, a pneumonia-like illness that defied treatments invaded Wuhan, China. Inside a month, it was identified as a novel coronavirus later known as COVID-19.]
Woodward

“The thing that stays with me is that overlying uncertainty. You take note of it, but you’re thinking, ‘Will it come to Mississippi?’”
Jones

“There were colleagues of mine, ER doctors in China, that part of the world, and they said, ‘This is real.’
“By February or the beginning of March, COVID was spreading through Italy and then to New York.
“We thought, ‘This is going to overwhelm the systems.’ And then, seeing all the COVID tents with patients in New York – that was surreal. …
“It may have been the last Sunday of Spring Break, in March, when we holed up in the VC conference room and started the intense work of preparation.”
Wilson

“We had planning in place based on the Medical Center’s response to other emergencies such as hurricanes or tornadoes, or on lessons learned from the [2014] Ebola outbreak or in planning for an influenza pandemic.
“But those scenarios were built around a one-time spike. COVID came in waves.
“A friend of mine in Homeland Security told me we should prepare for a 30-month response. I had been thinking of this like it was a storm: If we sheltered in place, it would blow over and we would come out on the other side. But that’s not the way it was meant to be.
“I don’t know if I had a time frame in mind, but I sure wasn’t expecting 30 months. Of course, my friend was right.”
Dobbs

“We had millions of masks in the warehouse, but that didn’t last very long. The supply chain, including PPE [Personal Protective Equipment] and ventilators, became its own drama.”
Wilhelm
“I told the nurses, ‘You've prepared your whole lives for this. And there's no one else I would rather go into this with.”
Woodward
“It seemed like we all had that feeling: ‘I’m not sure I know what I’m doing. Am I doing it right?’
“Like everyone else, I was also worried: ‘Am I taking something home to my family and is it dangerous?’
“The truth is, it was. But we were all in the same boat. Everybody was at risk. And we were willing to take that risk.”
Jones
“The Medical Center became the only place in Mississippi doing clinical trials or coming up with new therapies. We had a website sharing all our protocols. We developed an inhouse test and did all the testing for MSDH.
“We did everything we could do to be a state asset. And we were trying to manage when many of our own employees were sick.”
Dobbs
“Early on, Mississippi did a good job restricting gatherings. We shut down, and didn’t have many deaths.
“Pretty soon, though, people were tired of COVID. By Memorial Day, we started behaving really recklessly. People died who didn’t have to.
“We just watched it happen like a slow-motion train wreck, with people refusing to get off the tracks. We were trying to figure out the boundaries of our authority: ‘How far would you go to save someone’s life?’”
Wilhelm
“All sorts of measures were in place to keep the virus from getting outside the ICU, such as negative pressure. But some patients were getting delirious, trying to pull out the tracheal tube or trying to roll out of bed, and the nurses saw it and didn’t have time to put their masks on. They threw the door open and they ran in.
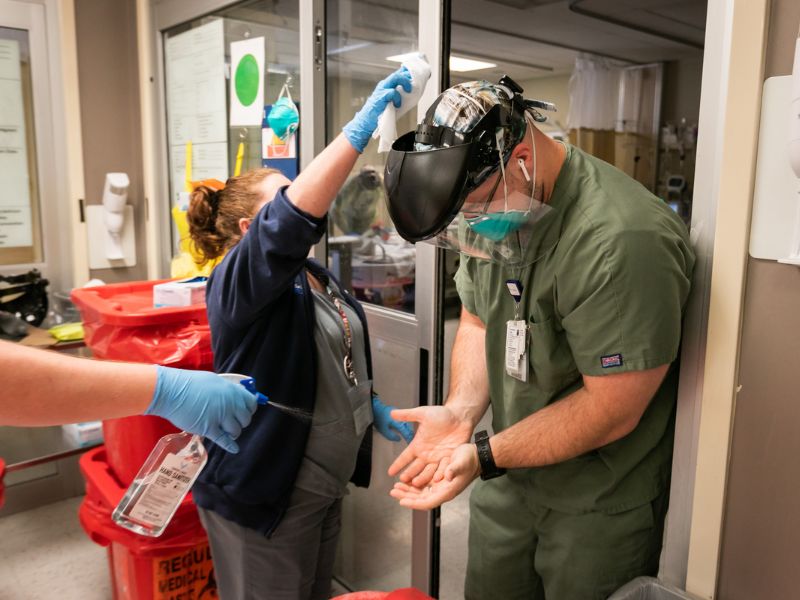
“And I remember grabbing someone by the back of the collar and yanking them back outside and saying, ‘You can't do that. Put your stuff on. We need you.’
“They were just trying to save people.”
Wilson
“When the media reported that they were digging mass graves in New York City for nursing home patients who had died of COVID, we realized that our morgue here was too small.
“So, we ordered two 18-wheeler trailers, morgue trailers. It was like I was admitting defeat, that I knew I wasn’t going to win. Thankfully, we didn’t have to use them. But it was such a low point.”
Wilhelm
“One particular patient I’ll remember forever: He was in the ICU and I was just watching him deteriorate. I walked into his room, and he just looked up at me in his bed right before I intubated him and said, ‘Don’t let me die. Don’t let me die.’ And all I could say was, ‘I’m going to do the best I can.’
“He died that night. …
“There was another patient, an older gentleman on life support. My team called his wife and she said, ‘COVID doesn’t exist. It has to be something else.’
“I said, ‘Ma’am, I wish it was something else. But your husband is dying. If you want to see him, now is the time. I don’t think he’s going to survive.’ She hung up.
“The man died alone with his wife denying that the disease that killed him even existed.”
[In April 2020, to prepare for an overflow of patients, the Medical Center set up a mobile field hospital in Parking Garage B.]
Jones
“That was crazy. Putting patients in a tent in a garage. It was like an out-of-body experience standing in that garage. You felt like you were in an unwinnable battle.
“Were you just chasing a mirage of a finish line?”
Wilson
“I thought, ‘Am I really doing this?’”
Dobbs
“It would have been impossible to navigate the pandemic without UMMC. It was a state leader in many ways. Dr. Woodward was really powerful in driving the thought processes around COVID.
“The Medical Center was the referral center for the sickest people, managing large numbers of critically ill patients.
“And, we would have had so many more deaths without the management of MED-COM for the system of care, which is like air traffic control for patients to get where they can get the care they need. That was enormously important.”
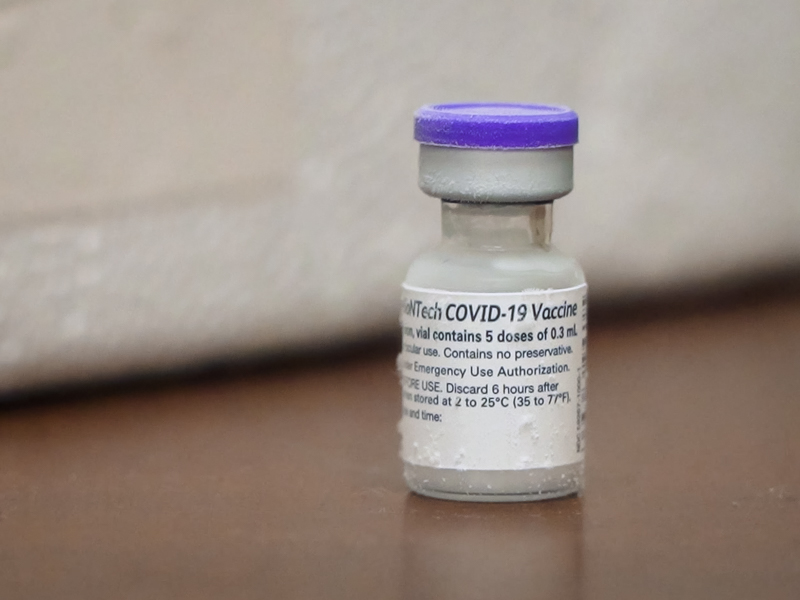
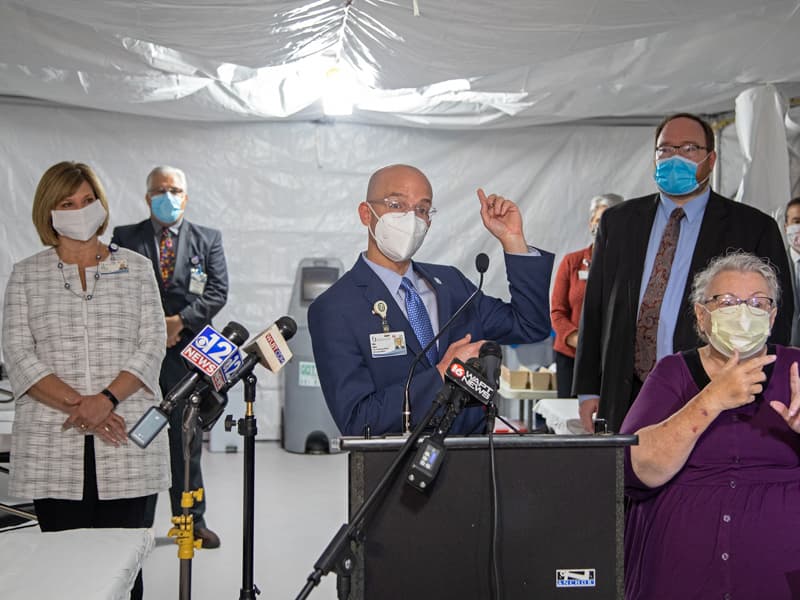
[In mid-December 2020, UMMC received its first allotment of the Pfizer COVID vaccine.]
Woodward
“Now, we had a tool. It was a different era in this fight.”
Wilson
“It was pretty powerful, the realization that it would make some of this go away. We didn’t have much hope before that.”
Jones
“I thought, ‘Maybe this is it.’”
Dobbs
“After the vaccine, very few people in nursing homes died. The number of deaths plummeted. After the first wave of vaccinations and the winter onslaught, there was a period of hopeful but anxious waiting.
“But, then, in the summer of 2021, there was the Delta surge.”
Woodward
“You’d see an improvement in the number of cases, then a new variant would break out.
“You can keep a certain level of adrenaline going only for a certain amount of time.
“I believe 95-plus percent of our employees wanted to answer the call, but after a year, it was ‘How long can you keep the energy up, keep people from being discouraged?’”
Dobbs
“The most depressing part of it all: Many people refused to take the vaccine. They died for no good reason.”
Wilhelm
“We ran out of body bags and were putting people in trash bags – one over the person’s head and one over the person’s feet and zip-tie them together. No one should ever have to put another human being in a trash bag.
“We lost some nurses – they said, ‘I just can’t do this anymore. I’m going to go do something else.’ More than once, I saw nurses sitting and crying.”
Jones
“I felt personally responsible for everything that happened clinically. You never felt caught up.”
Woodward
“If you only thought about the hugeness of it, you could go into a deep, dark place.”
Wilhelm

“You’re at the bedsides of people with different faith backgrounds, different ethnic backgrounds, all walks of life. But we’re all the same.
“You look at someone right before they die and all you can say is, ‘I’ll do the best I can,’ and they look back at you with the same eyes as everyone else when they’re staring at death.”
[In August 2021, in response to the Delta variant, UMMC opened a second field hospital, in Parking Garage C, staffed by Samaritan's Purse.]
Dobbs
“What helped sustain me was UMMC’s leadership and [MSDH’s] strong partnerships with other really committed people – health systems and hospitals, education systems, community health centers, faith-based organizations.”
Woodward
“You had to keep thinking of things like the homemade masks a church brought in. People who volunteered to bring in unused masks.
“We tried to keep non-clinical students at home so they wouldn’t get sick, but learned pretty quickly they weren’t going to do that. They wanted to be part of the drive-through testing, making test kits. Volunteering to serve as translators for patients, or dog-sitting for nurses who were at work, or building whatever needed building.
“Those were moments of inspiration for me.”
[Although there would be other COVID waves and variants, by the spring of 2022, the disease seemed under control, and things were opening up.]
Wilson
“There was never a point where it was obvious that it was about to disappear. It just kind of faded away, and we had a new state of normal.”
Wilhelm
“The mortality rate from COVID at UMMC was the same as it was for the rest of the country, even though our patient population is sicker, which increases the likelihood of dying.
“It doesn’t take away the pain of the losses, but I realize we did a pretty darn good job.”
[As of early this month, 1.22 million people in the U.S. had died of COVID including more than 16,000 in Mississippi. The lessons learned from the pandemic extend beyond the hospital bed, but not to everyone.]
Dobbs
“Even to this day, you’ll see social media posts saying COVID didn’t happen. Or that it wasn’t that bad. But a million people died in this country, and they died from something.
“A large portion of this country has induced amnesia. It was the deadliest thing that happened in almost a century and many of us are pretending it didn’t happen.
“But I do think we know how to respond better if it happens again.”
Woodward
“I don’t think we’re prepared for the next pandemic. Because we’ll have one.
“But we came out of it stronger than before, and I am proud of the response the Medical Center had.”
Jones
“It has changed me and the Medical Center for the better. It’s also comforting to know that you can personally overcome those challenges and work with people who have that same sense of resiliency.
“We learned a lot about their willingness to work together for a cause greater than the Medical Center, to let the responsibility of statewide health care sit on our shoulders.”
Wilson
“Every time there was a new wave, I went back to our core values: We take care of our patients, staff and employees. Always remember why we’re here.”
Wilhelm

“Seeing my team leave it all on the field and knowing we were taking arrows and darts from people who have never been inside the arena, seeing people standing on their personal rights, even if it affected whether someone else lived – that left me angry for a long time.
“But I didn’t want to stay angry forever. So, it was ‘How can I learn from this?’ I realized that you see people’s true colors when they’re under stress, that people react in different ways, and we have to figure out how to work with that.
“But I just want people to learn from all this. Because it’s going to happen again. And I don’t want all those people we lost to have been lost in vain.”


