Care team communication breakdowns aren’t healthy, happy

When a front-line caregiver is constantly at the bedside of a fragile patient, getting to a computer or cell phone to read a manager’s email or a campus-wide memo doesn’t rank.
When a patient is ready for discharge and needs rehab or a nursing facility, providers must get the word to social workers and case managers so that they can make arrangements in advance.
And when two departments plan an activity and each thinks the other is providing the refreshments because no one really talked about it, there are no refreshments.
They’re examples of potential communication breakdowns between teams and departments that can happen at the Medical Center, some with greater consequences than others.

“One of our biggest missteps is not taking the time to make sure our messages are received and understood,” said Vickie Skinner, director of UMMC’s Continuing Health Professional Education. “We deliver it, but we’re not sure if it was received and understood. We’re doing half of it.”
It can especially be exacerbated when the communication breakdown is between departments or areas of the Medical Center that don’t regularly work in tandem. And, communication breakdowns can prove deadly if caregivers don’t communicate and the patient gets the wrong medication, or surgery on the wrong site.
“It’s a major safety issue in health care,” said Chief Medical Officer Dr. Michael Henderson.
“The collaborative part we have a hard time with is working together to communicate. We have our own silos,” said Shayne Boackle, manager of ambassador services and educator for imaging services. “Sometimes, we don’t communicate as a group.”
Boackle and Skinner are among a group of Medical Center employees presenting “Divided by a Common Language: Navigating Communication Breakdowns in Healthcare,” an interprofessional education seminar sponsored by CHPE and the Associated Student Body. Set for noon-1 p.m. Oct. 30 in the School of Medicine Room 124, the seminar offers continuing education credits and features a panel discussion led by a cross-section of employees ranging from social work to pharmacy to dentistry to family medicine.
They’ll lead their audience in a discussion about common communication breakdowns in an interdisciplinary health care world and how to promote a culture of getting your message across in a format that’s good for both the sender and the receiver.
Skinner brings a unique perspective to the discussion. She’s a 24-year U.S. Army veteran with the rank of lieutenant colonel and also is a medical service officer. During two decades in the Army’s medical arena, Skinner spent several years in charge of a Fort Benning, Ga., base clinic that medically mobilized and demobilized more than 300 soldiers daily, with staff juggling lab testing, immunizations, eye and hearing screenings, pharmacy and physician visits, among other duties.
“The military has taught me bottom-line up front (BLUF) communication – always start with the bottom line up front,” Skinner said. That’s especially useful when sending email, she said.
“If we didn’t follow BLUF, we couldn’t have been as efficient and effective in delivering care at that hectic pace,” Skinner said of the military clinic, which ran from 6 a.m.-8 p.m. “I think we do this now, in areas like the Emergency Department, where time is critical.”
Most people will agree: There’s something to be said for in-person communication in health care, but if it has to be electronic, make it succinct, and be confident that it’s going to be received and read.
“In a health care system of this size, there’s not just one appropriate route of communication,” Boackle said. “Sometimes, people don’t have time to read the fine print, or to read emails that are from their manager. People say, ‘We didn’t know about it. We didn’t get that information.’ “
Compounding that is a millennial employee population accustomed to communicating primarily by text and email. “The young ones have not been taught to have a conversation face to face,” Boackle said.
“Our biggest challenge is that people forget that communication is an exchange of information, and not just the one-directional ‘I’m telling you something,’” Skinner said.
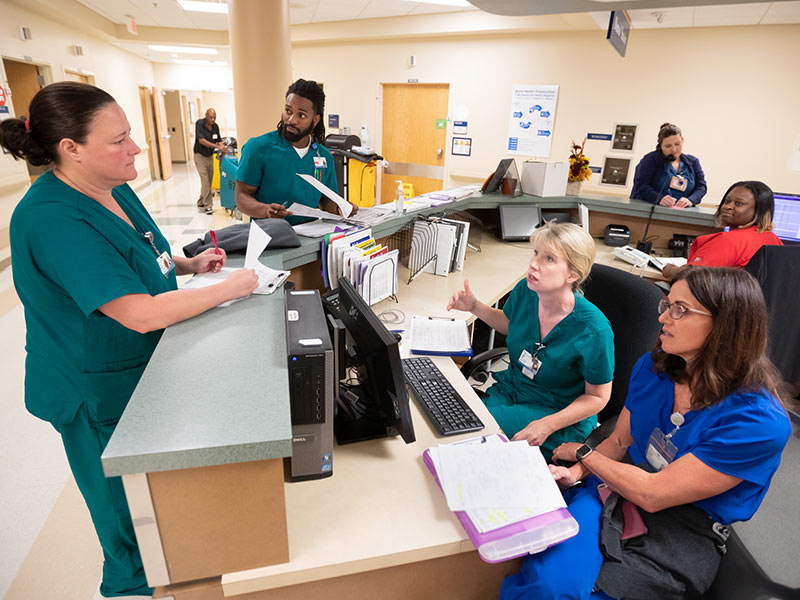
Two-way communication that spans multiple departments, however, is the norm and the rule under the guidance of Marina Baldwin, a nurse manager on 3 North in University Hospital. She holds a daily meeting that brings in nurses, case management workers and social workers to discuss care plans for the floor’s 32 patients.
That’s in addition to a multidisciplinary meeting at 10 a.m. each Monday and Thursday attended by nurses, case managers, social workers, therapists, providers and benefits staff. “We fill in the gaps and communicate with each other,” Baldwin said. “What do we need to do for this patient for discharge? What is the treatment plan? What is the recommendation for therapy equipment? Who in the family deals with Grandpa? What is his payor source?”
Sometimes, there’s no time for a scheduled meeting, said Todd Dear, the Medical Center’s director of pharmacy who also is a panel discussion member.

“We have challenges daily with several hundred drug shortages,” Dear said. “We have to have really quick communication with doctors and nursing staff and supply chain partners, and we have situations where we have to coordinate with people that we usually don’t coordinate with. We ask, how does that impact the patient? If we are short on a drug, who do we allocate what we have to?”
Communication problems can happen easily “because each challenge is different,” Dear said. “We’ve talked about establishing communication flow charts on drug shortages, and to have a best practice so that when you’re running between meetings and putting out fires, we can remember the communication lessons that we’ve learned.”
Unfortunately, it’s not unusual for many in health care to speak a common language, but fail to communicate through it, Skinner said.
“We need to take time to see each other face to face. Time is the barrier,” she said. “We don’t take enough time to sit down and look at each other.”
On a recent afternoon, Baldwin made time to chat with physical therapist Brandi Alexander and occupational therapist Randy Khalaf as the therapists gave care to patients on 3 North.
Alexander doesn’t see their twice-weekly gatherings as just another mandatory meeting. It’s so much more.
“It gives you a face to talk to,” she said.


