Brain studies examine role of hippocampus in autism, substance abuse
The hippocampus plays a major role in memory processing, and researchers at the University of Mississippi Medical Center are learning more about the myriad roles the complex brain structure plays in autism and substance abuse disorder.
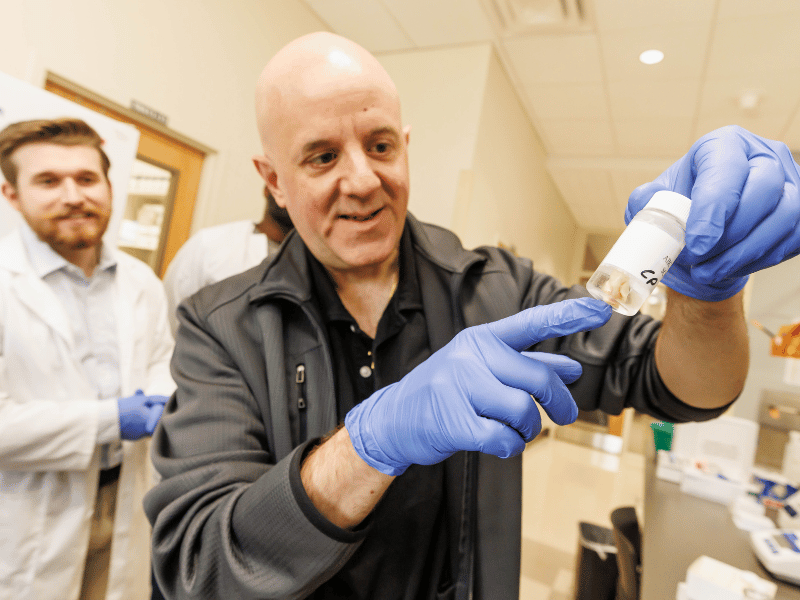
Dr. Harry Pantazopoulos, assistant professor of psychiatry and human behavior, and a team of researchers published two studies in February that have promising implications for the treatment of both disorders, which affect hundreds of millions of children and adults.
“The autism study is the first examination of the molecular processes that are altered in the hippocampus of children with autism spectrum disorders,” said Pantazopoulos. “This allows us to identify processes that may contribute to altered brain circuitry in autism and identify targets for preventative and therapeutic strategies.”
The developmental disability, characterized by social interaction impairments and repetitive patterns of behaviors, can result in difficulties communicating, learning and engaging in a wide range of daily activities.
About 1 in 36 children were diagnosed with ASD at age 8 in 2020, according to a Centers for Disease Control and Prevention report; the prevalence has increased substantially since 2000, when only 1 in 150 were diagnosed.
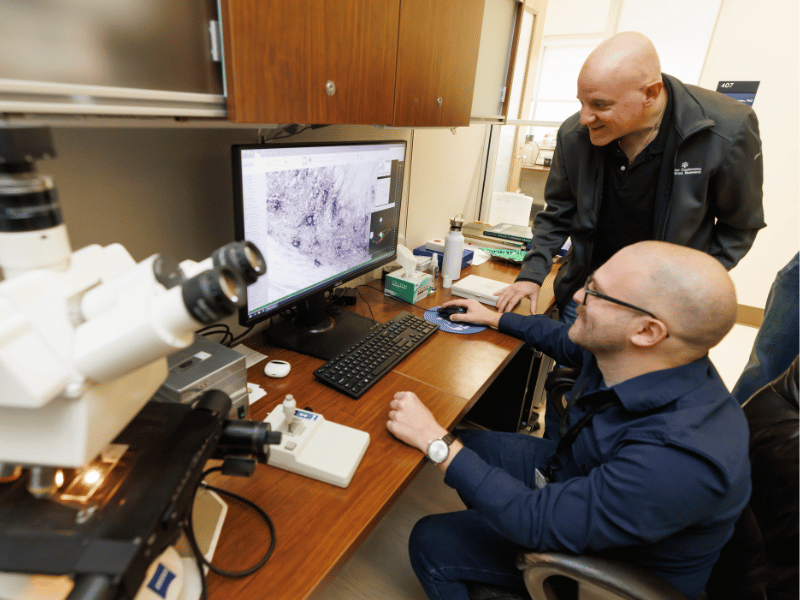
The findings uncovered in the article, “Molecular profiling of the hippocampus of children with autism spectrum disorder,” published in Molecular Psychiatry, zeroed in on a set of molecules called extracellular matrix molecules, that impact brain development and the immune system, representing a link between immune system dysfunction and neurodevelopment that can contribute to circuitry changes in the brains of children with autism in the early stages of development, Pantazopoulos said. Some of those molecules, which have been implicated by genetic studies of autism, may represent consequences of genetic factors.
“The hippocampus is a brain region involved in storing environmental memories and integrating these memories with emotional processes, so molecular alterations in this region during early life brain development may impact several aspects of autism,” Pantazopoulos said.
The study contributes to the idea that neuroplasticity, the ability of the brain to change and rewire itself, can contribute to the complex scope of autism, said lead author Lindsay Rexrode, a third-year medical student.
“The fact that we could pinpoint such pathways has pioneered many routes that can be explored, thoroughly understood and translated into clinical research,” she said.
Pantazopoulos, also director of the Postmortem Brain Core in the Division of Neurobiology and Behavior Research Program in Neuroscience, has long sought to understand the developmental brain process that contributes to autism to identify candidates for preventative and therapeutic strategies. The study was finally made possible by teaming up with the UMMC Molecular Center for Health and Diseases.
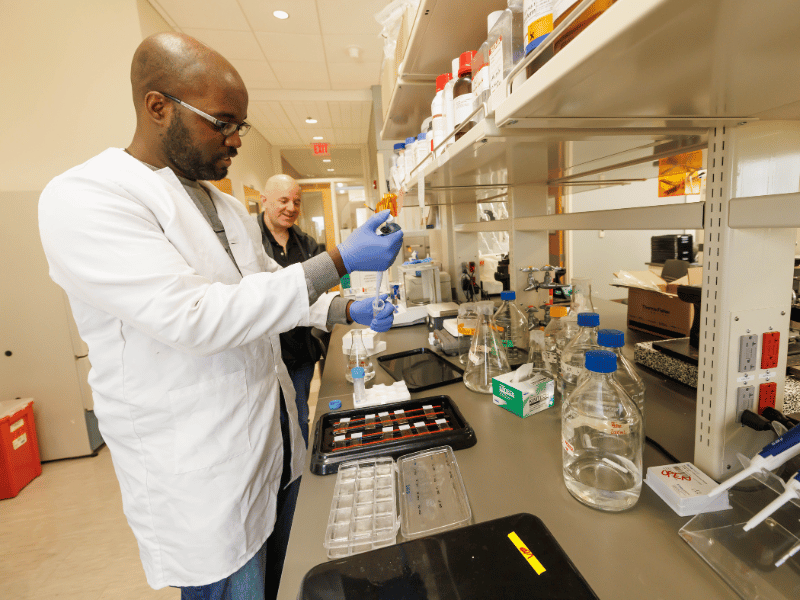
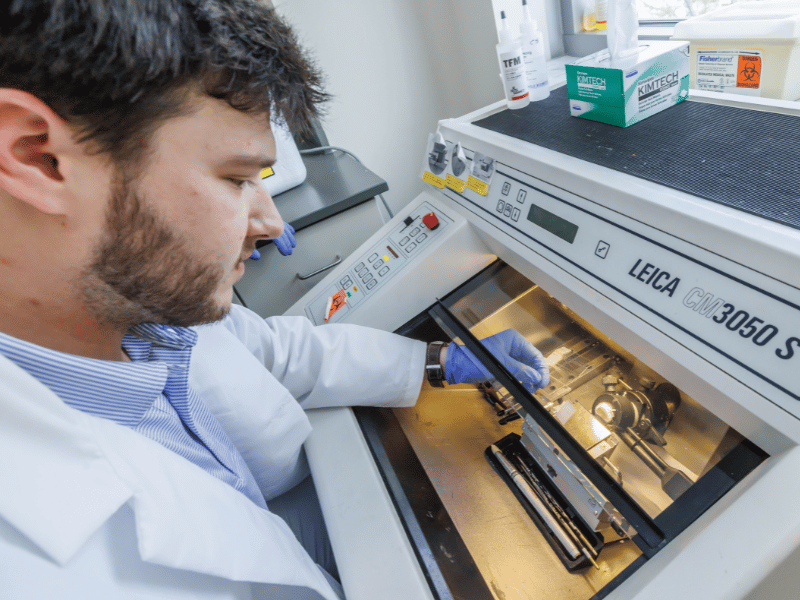
Substance use disorder is another disease he’d wanted to examine for a while. Published in Translational Psychiatry, “Extracellular matrix abnormalities in the hippocampus of subjects with substance use disorder” illuminates changes in perineuronal nets, brain structures that envelop certain neurons and strengthen the current connections those neurons make. This study was made possible with a unique collection of brain samples from the UMMC Postmortem Brain Core established by Dr. Craig Stockmeier, professor emeritus of psychiatry and human behavior.
“In essence, they hard-wire brain circuitry,” Pantazopoulos explained. “Our data, together with prior evidence from animal studies, indicates that drug use causes these structures to increase around neurons to strengthen drug reward memories, contributing to the difficulty to recover from substance use disorder.
“The hippocampus is a key brain area involved in contextual memory storage. Increases of perineuronal nets in this brain area are likely to contribute to the strengthening of contextual memories associated with drug use, and in turn to the process in which environmental cues trigger relapse. Thus, perineuronal nets represent a potential therapeutic target to weaken drug reward memories.”
There were no previous studies focused on the perineuronal nets in the human brain of patients with substance use disorder, said Jake Valeri, a research assistant and student in the PhD in neuroscience program and lead author of the article. The team used UMMC’s human postmortem brain bank, which includes substance use disorder specimens.
Valeri, who’s worked in addiction clinics, saw firsthand the number of people who would leave the clinic, only to return after relapsing, many with a strong desire to quit long-term.
“Upwards of 60% end up relapsing multiple times after receiving treatment,” Valeri said. “Once I was lucky enough to work in a neuroscience lab during undergrad, I learned that most of the classical ways we currently treat substance use disorders do not treat an underlying pathology. I knew from here that if we wanted to make more efficacious treatments for SUD, we first had to more deeply understand what was happening in the brain.”
According to the National Survey on Drug Use and Health, more than 46 million people aged 12 or older met the criteria for having a substance use disorder in 2021, with the highest prevalence among young adults between 18 and 25.
The study is significant because it helps uncover some of the biological traits linked to high relapse risks, said Valeri, who was particularly interested in the research because he’s had several friends struggle with addiction. “A guiding hypothesis for future studies based on these findings is that you could potentially better prepare people following rehab against relapsing by prescribing a medication that targets the extracellular matrix.”


