Study: Single clinic visit can help thwart HIV infection spread
One clinic visit - just one - can make a significant difference in young black men who have sex with men protecting themselves from contracting or spreading the HIV infection, a national study co-investigated by a University of Mississippi Medical Center expert concludes.
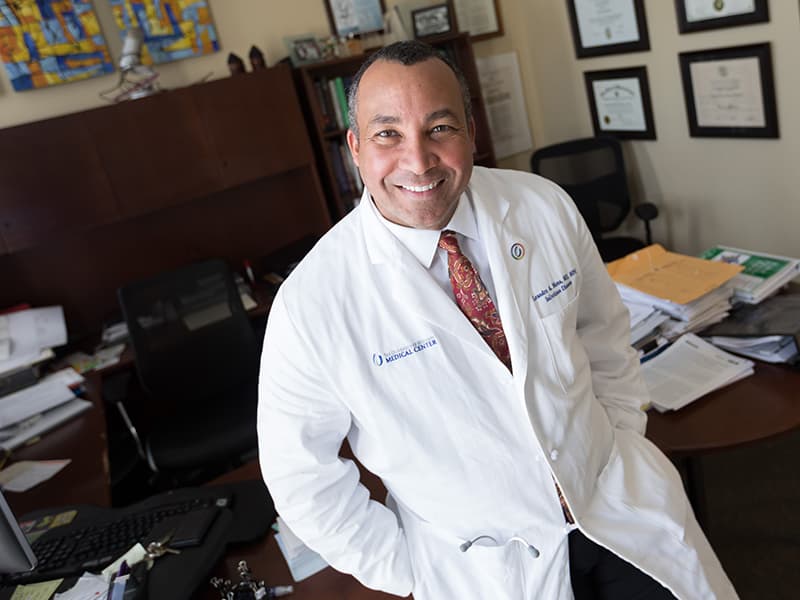
The findings have huge national implications in controlling the potentially deadly virus at a time when sexually transmitted infections have hit a national all-time high, said Dr. Leandro Mena, professor of infectious diseases and population health and chair of the Department of Population Health Science in the John D. Bower School of Population Health.
“This will be of great interest to many working in this field in the nation,” Mena said of the more than $2 million study funded by the National Institutes of Health and the first of its type nationally. “It’s very possible that it may become one of the evidence-based (treatment) interventions disseminated by the Centers for Disease Control and Prevention.”
In the study and its publication that Mena says is perhaps the most important of his career, Mena and Dr. Richard Crosby of the University of Kentucky co-investigated a randomized, controlled clinical trial in which 600 young black men in Jackson who have sex with men, YBMSM for short, participated and were encouraged during a single STD clinic visit to use condoms to prevent HIV infection.
The men were observed over a 12-month period that took place between 2012 and 2016, with the STD clinic visit-driven intervention culturally tailored to the Jackson area.
The results, first published online in the Journal of the American Sexually Transmitted Diseases Association, showed the HIV-infected Jackson men who went to a single clinic visit were 64 percent more likely to report they’re using condoms during anal sex. HIV-negative men in the same intervention group were more than twice as likely to report consistent condom use 12 months after receiving the intervention, compared with controls.
“This is clearly a program that can be used not just in Jackson, but in any population in the Deep South,” said Crosby, an endowed professor in the University of Kentucky’s School of Public Health and an adjunct professor at UMMC.
“Nationally, Jackson has the nation’s leading rate of AIDS diagnosis,” Crosby said. “It’s a very important place for work like this, because the goal is to find where an epidemic like HIV is the worst, and intervene there. Jackson has one of the worst (STD/HIV) epidemics in the country.”
The study is a call to action for increased federal funding for STD clinics in addition to the STD operations at the CDC, said David Harvey, executive director of the National Coalition of STD Directors.
“This speaks to the importance nationally of supporting STD clinics,” Harvey said. “These services are the forgotten stepchild of the public health system. We need to change this.”
Also of huge importance, Crosby said: About one-third of the men studied already had one or more STDs, not including HIV. Nationally, Mena said, Mississippi leads the nation in gonorrhea rates, is third for chlamydia and seventh for both primary and secondary syphilis.
More than two million cases of chlamydia, gonorrhea and syphilis were reported in the United States in 2016, the highest number ever, the CDC announced Sept. 26.
One in seven Mississippians who have the HIV infection, or about 15 percent, don’t know it, the CDC says. Of those aged 15-24 who have HIV, more than half don’t know it. The continuing concerning news is that Jackson has the fourth-highest rate of HIV diagnosis per 100,000 population among the nation's metro areas. Overall, an estimated 10,300 Mississippians are living with HIV – but that’s only the diagnosed cases.
“Increases in STDs are a clear warning of a growing threat,” Dr. Jonathan Mermin, director of the CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, said in a news release. “STDs are a persistent enemy, growing in number, and outpacing our ability to respond.”
Both Harvey and Fred Wyand, director of communications for the American Sexual Health Association, are grateful for studies that reveal the benefits of interventions that can be provided through STD clinics.
“If there is data that indicates a single clinic visit has an impact, it’s worth getting the word out,” Wyand said. “That’s a fairly minimal intervention with a high payout.”
“Any research of this nature is desperately needed to show what a difference STD clinics can make,” Harvey said. “We don’t have enough research done. This study really shines a light on a national problem. We need more research studies just like this one.”
The study, to be published in print in October, “has produced almost two dozen publications that have significantly broadened our understanding of the HIV epidemic among young black men in our region,” Mena said. “And we’re talking about a one-hour clinic intervention.”

