Taking up residents: Projects pursue greater doctor relevance, well-being
Imagine scaling the Matterhorn when all you’ve ever climbed is a mimosa tree. Imagine driving the Daytona 500 when all you’ve ever raced is a Vespa.
In either case, you’re likely to become overwhelmed and frustrated: feelings that are, if not quite as exaggerated or profound, are at least similar to what physicians can experience in a setting for which they aren’t prepared.
So imagine a program that addresses this problem before it occurs – that is, during training – and you have the Reimagining Residency Initiative, an emerging effort to help medical students move “safely” into specialty training, and then, as specialists, into practice as fully-fledged physicians.
In this push toward greater relevance, the University of Mississippi Medical Center is playing a major role as the co-recipient, with Vanderbilt University Medical Center, of one of eight, five-year $1.8 million grants for projects conceived to change the landscape of residency training.
“Well-being, for physicians, is a great emphasis in these grants,” said Dr. Jimmy Stewart, UMMC professor of medicine and the associate dean for Graduate Medical Education.
“It comes down to professional development and identity. With our grant, it’s all about shooting for the moon.”
This moonshot, one of 250 proposals submitted, comes with a title: the GOL²D Project (Goals of Life and Learning Delineated), one of the proposals accepted and funded with a total of $14.4 million in competitive grants from the architect of the Reimagining Residency Initiative: the American Medical Association.

“Ideas came to us from residency training programs, hospital systems, physician organizations, partnerships across medical schools and more,” said Dr. Susan Skochelak, group vice president for Medical Education with the AMA.
“With these eight projects, we’re improving on what’s already good. There isn’t anything broken about graduate medical education. But we always know we can do better – especially in that area of helping physicians hit the ground running when they are ready to practice and work within the health care system.
“We also have important issues to address in trainee satisfaction. Physicians are quite stressed in this environment. We want them to have a lifelong approach to learning that keeps them satisfied and keeps them from burning out.”
In several studies, more than 40 percent of physicians in the U.S. have disclosed undergoing burnout, reports the Harvard Business Review.
The UMMC/Vanderbilt project “better prepares physicians to dodge burnout,” Stewart said. One key is the “five personae” feature, the result of Vanderbilt’s research. It’s an approach to patient care that prepares physicians to better meet challenges by developing or improving on these traits or roles:
- Competency, humility
- Creativity; curiosity about improving a process in ways that help patients
- Leadership and advocacy
- Familiarity with the workings of the health care system
- Master adaptive learner and teacher
A team effort between UMMC and Vanderbilt is a natural one, considering the strategic partnership that already ties together the two institutions, said Dr. Donald Brady, Vanderbilt’s senior associate dean for Graduate Medical Education.
“The two places have great complementary strengths,” Brady said. “Both are in states where health outcomes are not at the top of the country’s rankings. But both are very committed to improving the health of the pubic.”
All this begs the question, though: If residency training isn’t broken, as Skochelak said, why is it so important to orchestrate changes that, between UMMC and Vanderbilt, will affect about 1,700 residents and some 160 different programs?
“Health care has evolved,” Brady said. “Systems are changing. There are mergers, acquisitions, telemedicine. We believe there are certain skills that need to be taught that haven’t necessarily been taught in the past. And that other things at the core of the profession could be enhanced.”
Beyond that, Reimagining Residency did not pop up out of nowhere, like an uncultivated weed. It’s a sequel, of sorts, a follow-up to the AMA’s 2013 plan to transform medical education, starting with medical schools.
“[Reimagining Residency], in many ways, is a companion to what we did with medical schools,” Skochelak said. “In that earlier initiative the goal was to break out of the box of this very old and rigid design for training physicians.
“It added new content in the medical school curriculum on how the health system works. It has helped students focus on working in teams, on making sure the patient is at the center. It is about bringing the real world into medical education, including social determinants of health, patient safety and more.”
Social determinants of health: UMMC’s EversCare Clinic is already on that. Housed in the Myrlie Evers-Williams Institute for the Elimination of Health Disparities at the Jackson Medical Mall, the clinic connects patients to resources that help them cope with food insecurity, along with such needs as housing, literacy and transportation.
So, as a training venue, EversCare is ideal for endowing residents with many of the GOL²D’s physician personae, said Dr. Bettina Beech, UMMC professor and dean of the Bower School of Population Health.

“EversCare helps [residents] understand where action can be taken to help patients when the patients don’t know where to go,” said Beech, executive director of the Evers-Williams Institute and co-investigator, with Stewart, on GOL²D.
“The AMA has recognized that there is more to a well-rounded physician than competent clinic care, which is vital; but being a lifelong learner and an advocate for patients will round out the physician experience, and make it more comprehensive.”
While well-roundedness has been emphasized for 19,000 students in a consortium of more than 30 medical schools for several years now, it can’t end there, Skochelak said.
“Now, those medical students are graduating and going into residency programs. So the question was: Are they going to just fall off a cliff and not have these ideas reinforced in residency training?”
The creators of the GOL²D Project answer: No. This blueprint is meant to respond to a resident’s unique needs, while making training, overall, more relevant, Stewart said.
“If a physician wants to practice in Philadelphia, Mississippi, without any knowledge of the Choctaw community there, he or she may be an excellent physician, but won’t know how to deal with the community’s cultural beliefs.

“Or if a surgeon wants to pursue a career in hospital administration, say, in Meridian, he or she would have zero knowledge about doing that now. But this new training can offer an elective that delivers the information needed to succeed.”
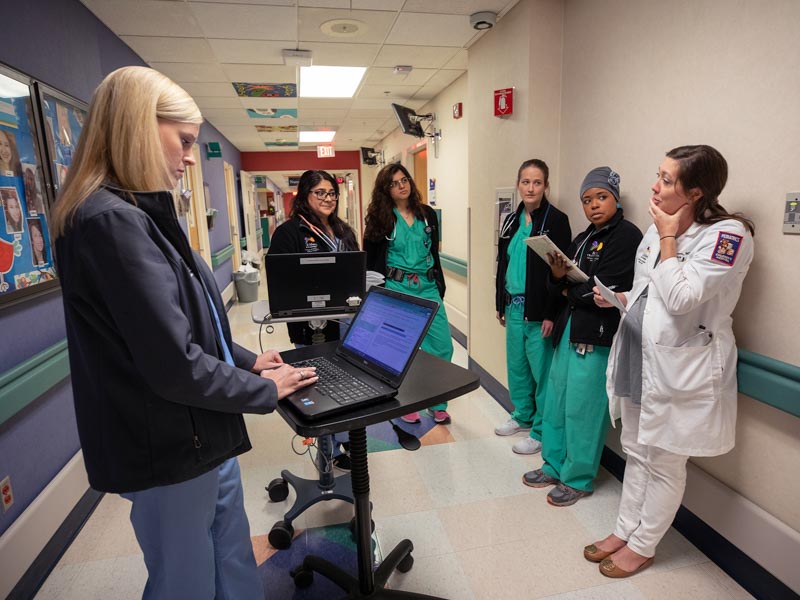
At UMMC, about 66 programs will adapt this tailor-made approach, involving some 640 residents and fellows, including Dr. Malorie Holmes, an internal medicine resident and graduate of Meharry Medical College in Nashville.
She’s looking forward it, she said. “It’s important to me that I receive the training and experience most pertinent to my specific goals in medicine.
“An individualized approach is certainly a more efficient way of producing competent physicians and a more effective way of prioritizing the well-being of medical students and residents.”
UMMC/Vanderbilt’s approach to residency training won’t be untethered, or lost in institutional space, said Dr. John S. Andrews, AMA’s vice president for graduate medical education, innovations.
“Principal investigators from all the eight projects we funded will hear about each other’s projects. They will try to agree on common goals and work in unison, making sure the transition from medical school to residency is seamless.”
They can borrow from each other, Skochelak said.
As for UMMC/Vanderbilt, between now and September, Stewart and Brady will organize their own campus groups to develop GOL²D, while staying in touch, through on-site visits or teleconferencing. At the Medical Center, department chairs and vice chairs, the Chief Residents Council and many others will weigh in, Stewart said.
Funding begins in August, but the two institutions will devote the first year of this five-year project to planning – understandably so, when you’re reaching for the moon.
REIMAGINING RESIDENCY GRANTS
The GOL2D Project (Goals of Life and Learning Delineated): Collaboration Across Academic Health Systems to Better Align GME with Learner, Patient and Societal Needs—Vanderbilt University Medical Center and the University of Mississippi Medical Center
California Oregon Medical Partnership to Address Disparities in Rural Education and Health (COMPADRE)—Oregon Health & Science University and University of California, Davis
Fully Integrated Readiness for Service Training (FIRST): Enhancing the Continuum from Medical School to Residency to Practice—University of North Carolina School of Medicine
NYU Transition to Residency Advantage—NYU School of Medicine
Promotion in Place: Enhancing Trainee Well-Being and Patient Care Through Time-Variable Graduate Medical Education—Partners HealthCare System, Massachusetts General Hospital, and Brigham and Women's Hospital
Reimagining Residency: Ensuring Readiness for Practice Through Growing Interprofessional Partnerships to Advance Care and Education—Maine Medical Center
Residency Training to Effectively Address Social Determinants of Health: Applying a Curricular Framework Across Four Primary Care Specialties— Montefiore Health System in New York
The Graduate Medical Training “Laboratory”: An Innovative Program to Generate, Implement and Evaluate Interventions to Improve Resident Burnout and Clinical Skill—Johns Hopkins University School of Medicine, Stanford University School of Medicine, and University of Alabama at Birmingham School of Medicine


