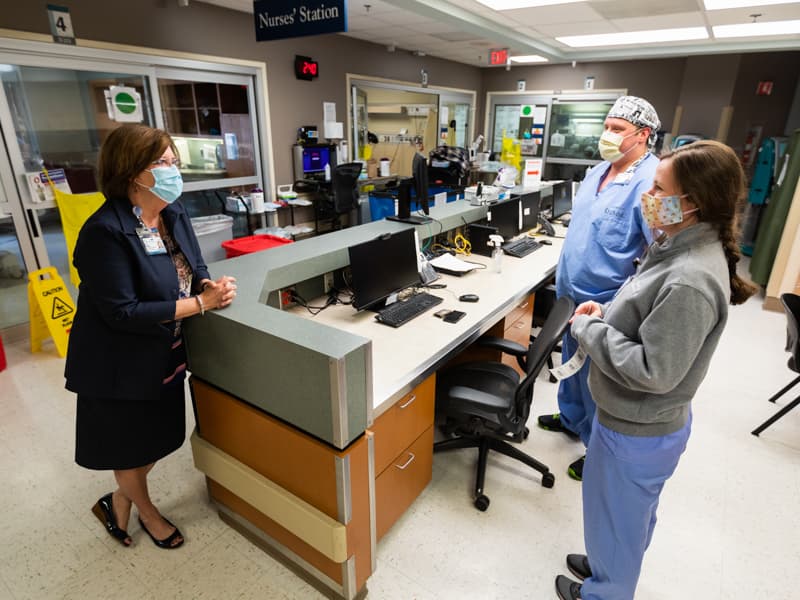
Health System keeps ship steady despite COVID-19's uncharted waters

As the end of May approaches, the University of Mississippi Medical Center’s COVID-19 patient population not only hasn’t peaked, but last week saw record highs.
It’s a landscape that is ever-changing, one that keeps the Health System’s leadership on a journey that’s exhausting and sometimes unpredictable, yet pride-filled.
Months before the front line cared for its first person stricken by the virus, leaders put into action plans to keep patients and 10,500 employees safe. For the duration of this pandemic, that will be the priority.
Lessons learned through the Medical Center’s response aren’t just guiding the present. They’re providing flexibility and resolve for the unknowns that lie ahead.
Kevin Cook, chief executive officer, Health System
“As we watched the news reports coming in from China, we knew there was the potential for something big, but I don’t think anybody could have anticipated what we are seeing right now,” Cook said. “We were dealing with something completely outside our experiences.”

His biggest concern “all along has been ensuring that the front line has what it needs to do their job safely,” Cook said. Still weighing heavy is the need for personal protective equipment to shield employees from a highly contagious and often mysterious virus.
“We started spending a lot of time focusing on our supply chain, and the realization early on that supplying our front-line providers could be a challenge,” Cook said. “We’ve stepped up to meet the challenge.
“My second concern was to make sure the right people were in the right places. People have stepped up,” Cook said. “I couldn’t be more proud of the entire leadership group at UMMC. Everyone has been asked to do things a little differently.”
Cook let Health System leaders know that they needed to pace themselves for a marathon and not a sprint.
“He immediately started talking about preserving yourself – not letting yourself get run down, and bringing in your number two to meetings so that when you get away from the hospital, there won’t be a drop-off,” said Dave Estorge, Cook’s chief of staff.
“I thought this was a strange thing to say during week one, but Kevin knew the trajectory we were on. He insisted that this group take care of themselves.”
Fast forward to today. “As we ramp operations back up, the supply chain will continue to be a focus, especially in looking at how much PPE we will burn through,” Cook said.
“I’m very proud of the work of the supply chain,” he said. “I’m confident that we can get the PPE that our front-line needs. But, I don’t think the challenges are going to go away any time soon. They will only escalate.”
Britt Crewse, chief executive officer, Adult Hospitals
As the virus invaded Mississippi, Crewse and his team consulted the Medical Center procurement staff on a daily basis. “They were following about 75 leads a day to completion, whether or not that resulted in us buying from any of them,” he said.

Executives and their teams brainstormed a plethora of new and creative ideas that made the Health System’s response that much more robust – and so did the Medical Center’s researchers and faculty.
Dr. Charles Robertson, a pediatric anesthesiologist, invented the Robertson ventilator. UMMC scientists created an in-house COVID-19 test.
“We beat almost every hospital in the country in developing that test,” Crewse said. “It usually takes months to validate a test. We were able to do that in two weeks, and we’ve been able to test more patients pre-surgery and pre-procedure, and to help hospitals across the state.”
In the hospital’s clinical enterprise, “we realized that when our volumes fell, the need for front-line personnel wasn’t as great as normal,” Crewse aid. “We quickly set up the UMMC Reserves under the leadership of Karen Dowling and others. It was very unique.
“We had to invoke a no-visitors policy in the adult hospitals. You went from open visitation to none. We did this within hours,” Crewse said.
Leaders also realized early on that large numbers of patients couldn’t come to clinics for critical lab work. The solution: Drive-through laboratory stations in which 100 patients a day can pull up in their vehicles, wait until they are called, then exit their vehicle long enough for a blood draw.
“It’s a different service model,” Crewse said. “We are learning from this crisis about how we can become better.”
The chemistry between leaders has made all the difference in fulfilling directives now while focusing on the job ahead, Estorge said.
“I thought we were a pretty close group before this started, but we’ve gotten very close and leaned on each other,” he said. “We’ve leaned into this.”
Terri Gillespie, chief nursing executive and clinical services officer
Gillespie’s wedding anniversary was March 6. “We went out to eat, and I said to my husband, ‘Based on what I’m hearing, this might be the last time we go out to eat for a while.’”
The next few weeks were “a flurry … Counting PPE and hand sanitizer. Putting into place plans to limit visitors. Putting together the crews to work at the front desk.”
At least 400 members of the Medical Center’s 2,700-strong nursing force are dealing directly with COVID-19 patients, Gillespie said. When she walks the units and floors, and sees them in action, “I’ve never been more proud to be a nurse.”
“When we got our first patient, there was a lot of angst,” she said. Nurses had not so much fears, but questions.
“Do I need to change clothes before I go home? We provided extra scrubs for that. Do I need to take a shower? We provided housing for that.
“We communicated all the things that we had done to keep them safe, and in two or three days, the doctors and nurses had it down to a fine art. They had it down to a science.”
She’s watched the nursing staff adapt to the personal and professional challenges wrought by the pandemic.
“Some are so young that they don’t have any memory of the Ebola scare a few years ago,” she said. “They might have read in textbooks about the Spanish flu. They have not shrunk away from this. They are very anxious to come and take care of these patients.”
Veteran nurses, she said, “are unfazed.”
Nurses “hold the iPad so that patients can FaceTime with their family. They hold their hand when things are getting worse. They are their lifeline,” Gillespie said. “They are their significant other.
“They are always with the patient when the patient dies, and they have seen a good many patients die, and die quickly.
“Our nurses have said, ‘If people could only see what we see.’ We might have COVID units for a long, long time,” Gillespie said. “But, there’s pride in that, definite pride. We’ve got this. We will keep fighting this battle.”
Guy Giesecke, chief executive officer, Children’s of Mississippi
COVID-19, statistically, has been less of a risk for pediatric patients, which has meant that Children’s of Mississippi leaders have been asking what they can do to help adult care at UMMC.

“Most children who have contracted COVID-19 did not have to go to the hospital, and they had mild symptoms,” Giesecke said of Children’s of Mississippi, UMMC’s pediatric arm. “Because of that, the state’s only children’s hospital has not been overwhelmed.
“That has allowed us to help the adult hospital by providing care for young adults in the children’s hospital. We’ve been doing that in the pediatric intensive care unit and in the medical-surgical units.”
Elective surgeries are now available, following the planning of pediatric leaders on how best to reopen for non-emergency procedures
“We’ve been looking at how to reopen in a way that will be safe for patients and would not put our care team members at risk,” Giesecke said.
Children’s of Mississippi’s outpatient specialty clinics have reopened to more than just essential care. With locations on the UMMC campus as well as in Tupelo, Hattiesburg, Meridian and Biloxi, most visits before May 4 were limited to telehealth visits, with only the most essential care done in person to limit the possibility of virus’ spread.
“Our specialists’ patients don’t need to go a long time without seeing their doctors,” Giesecke said. That includes cardiology, neurology, orthopaedics, endocrinology and pulmonology.
“We want children to have access to their physicians so they can have the best outcomes,” he said.
Dodie McElmurray, chief executive officer, UMMC Grenada and UMMC Holmes County
McElmurray early on juggled much more than COVID-19 patients. Just weeks after becoming the two hospitals’ leader, she managed a week-long water outage.
That was followed by a tornado that left much of the community without power for a week, including at the hospital’s off-site medical complex that houses outpatient imaging, cardiology and primary care.
McElmurray and her leadership team had to quickly prepare UMMC Holmes County, a 25-bed critical access hospital in Lexington, for an influx of COVID-19 patients in its Emergency Department and their transport to other hospitals based on the level of care needed.

“In a small hospital, you wouldn’t have ventilators,” she said. “But if you have patients coming in who need them before they are transported, then you do.”
Throughout it all, McElmurray said, she’s been in awe of her staff “and their ability to rise to any occasion they are handed.
“Leadership teams from both hospitals have come together to assist each other,” she said. “Our junior staff is learning from our senior staff. They’re trying to do what’s best for their patients, but also to keep their families safe, and that’s a real concern. But, they’ve never let it slow them down.
“In a small town, the community really looks to the hospital for its guidance,” McElmurray said. “That’s a role we play as well.”
Molly Brasfield, chief human resources officer
School closings left parents with kids at home. Employees had to quarantine or self-isolate due to COVID-19 exposure, travel during spring break, or because they or relatives fell ill.
“We knew people would have safety concerns, would be scared and worried, would be feeling uncertain,” Brasfield said. “We are holistic beings. If we feel stress in one area of our life, we can’t help but be affected in others. This was bound to create challenges to employees’ engagement at work.”
Her team “had a lot to think about and a lot to do,” Brasfield said. “But, many existing policies were already in place for this. It was the volume and context that were different.”
When HR needed guidance on changes to the work environment based on COVID-19, Brasfield said, “we relied so much on our own clinical leadership team. Other employers were using external resources for that, but we could leverage our own.”
Also top of mind for Brasfield and her team was the possibility of large numbers of front-line caregivers falling ill with the virus. Luckily, that has not been the case.
“We planned for the worst, and hoped for the best,” Brasfield said. “The success of the UMMC Reserves showed how we have resilient employees willing to be shifted and moved to really serve where we needed it most.”

She’s proud of her team, nurturing professionals who see their job as a calling.
“I’ve seen the same level of commitment across the UMMC leadership team,” she said. “The people of Mississippi are counting on us.”
The work ahead is daunting, and leadership will navigate more unknowns.
“Our biggest challenge is how to provide services in this new environment that are good for patients, and good for providers,” Cook said. “We’re going to reinvent portions of health care.”
Cook has assembled a group of operational and clinical leaders to do just that.
“We are getting the best thinkers in the room to address this,” he said. “Our teams are used to taking care of the sickest of the sick, and we handle things that no one else in the state handles.
“I’m enormously proud that we have continued to do that, and the thing I derive the most pride from is our front line. The community recognizes what we do on a daily basis.”


