New division to expand genetic testing as a health care force
It’s a familiar and tragic story: A young, apparently fit, athlete collapses on a football field, soccer pitch, basketball court or other arena – for no apparent reason.
Often, in the cases of sudden death, the reason turns out to be cardiac arrest, the upshot of a genetically decreed heart disease that had not been uncovered by routine screening.
Those deaths did not have to occur – if only the victims had known, early on, the potential risks of participating in demanding sports activities.
Yet, there is a way to expose such risks – not just for heart disease, but for cancer and other disorders as well – one that overcomes the limitations of standard screening measures, with a potential so far-reaching it has merited the creation of a new Department of Medicine division at the University of Mississippi Medical Center: Medical Genetics and Precision Medicine.

“We are at the end of the first inning, with a long game to be played,” said Dr. Javed Butler, referring particularly to medical genetics, a branch of medicine that applies the study of heredity to medical care, offering clearer paths for diagnosing and treating patients who have certain inherited disorders.
“It will evolve tremendously over the next 20 years,” said Butler, professor and chair of the department and the Patrick Lehan Chair of Cardiovascular Research. “The real work starts now.”
Much of the work starts with the newly appointed division director, Dr. Joe Maher, a hematologist and professor of medicine, whose current practice has been focused on hereditary cancer and other disorders such as hereditary aortic aneurysms, which can be life threatening.
Some of his patients have breast cancer, which, in a small percentage of cases is hereditary and is associated with inherited gene mutations. Genetic testing can expose the mutations early on, which, of course, could save patients’ lives.
Lately, genetic testing has “almost exploded” in scope, said Maher, whose division becomes one of more than a dozen in the Department of Medicine.
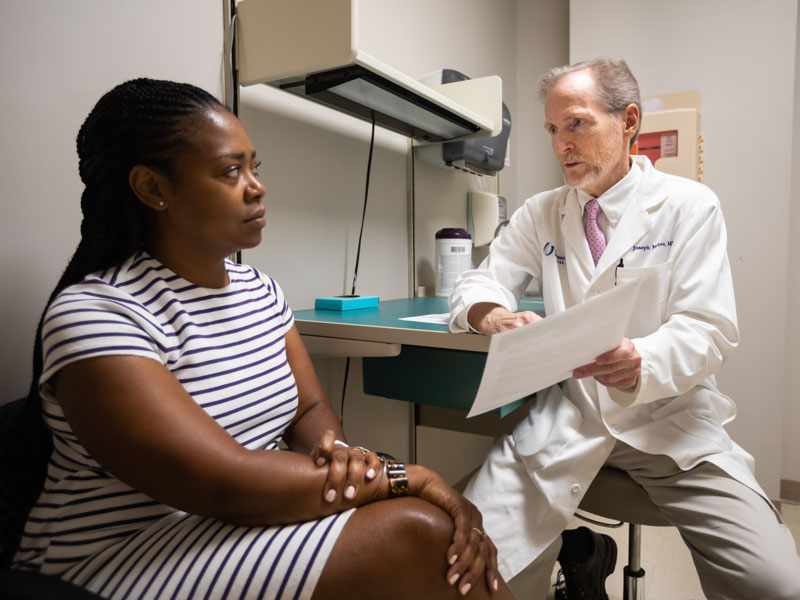
“Genetic testing can pinpoint and confirm a diagnosis,” said Maher, who sees patients at the Jackson Medical Mall, also the site of the division’s clinical work.
It can help physicians diagnose a patient early, before symptoms set in, he said. It can help them prescribe preventive measures for those who inherited certain gene mutations that can lead to disease. It can point to those family members who inherited a certain mutation – which occurs when the DNA making up a gene becomes damaged. It can also determine who did not.
Testing is, of course, not limited to patients at risk of heart disease or certain cancers.
“There are more than 5,000 genetic disorders that can be tested for right now,” Maher said. “We can say now, for sure, whether someone’s offspring inherited a gene disorder. We don’t have to guess. It’s no longer 50-50.”
As the name of the division suggests, medical genetics’ health care partner is precision medicine, a relatively new approach to disease treatment and prevention that considers not only inherited traits, or genetic makeup, but also other factors, including a patient’s lifestyle: smoking, drinking, exercise and so forth.
It offers physicians and researchers a way to more accurately predict which measures for treatment and prevention will work on a particular disease – and with which patients.

“The pace of discovery of new treatments is far faster than any physician is able to keep up with,” said Dr. John Ruckdeschel, director of the UMMC Cancer Center and Research Institute and Ergon Chair in Cancer Research.
The work of Maher and the new division will “help physicians sort out what makes sense for patients,” Ruckdeschel said. “It’s about having one location where this can be worked through and where physicians can go to for advice.”
Patients who come to UMMC for cancer treatment, for instance, “don’t need one doctor,” Ruckdeschel said. “They need a team.” Maher’s division can help the members of the team deal with a patient’s specific medical issues.
As for one certain issue, both Ruckdeschel and Maher use as an example the breast cancer gene BRCA1. Confusingly, because of its name, BRCA1 does not cause breast cancer, but can actually go a long way in preventing it. But if this gene mutates, it may lose its power to do so. Anyone who has this mutation, which can be detected through genetic testing, should begin breast cancer screening at age 25, Maher said, “and, at some point, consider preventive surgeries.”
As for precision medicine, one of its beauties is that it could help physicians more effectively treat their patients’ tumors, which aren’t inherited but which have genetic changes that cause cancer to grow and spread. They can learn whether a tumor will respond to a particular treatment. Or whether the risks posed to the patient by the therapy are worth it.
Some cancer treatments are toxic to the heart, Maher said. “But one patient may experience fewer adverse effects than another.” Dosages could be adjusted accordingly. This is an aspect of precision medicine known as pharmacogenomics, the study of how genes affect a patient’s response to drugs; it can lead to the development of effective and safe medications that fit a person’s genetic makeup.
“In the long run [medical genetics and precision medicine] can save a lot of resources,” Maher said. That means, for one thing, less time will be wasted on unnecessary treatments. Safer, and more effective, ones will be pinpointed, and sooner.
But, because of the “newness” of this knowledge, particularly medical genetics, Butler said, “not a lot of people around the country are trained in it. So people who need these services aren’t getting them, not only because of that, but also because many physicians don’t realize their patients can benefit from them.”
So the new division will serve as a “hub” for increasing knowledge about ways subspecialists can be more effective for their patients. For now, the division will begin building staff, putting in place a genetic counselor and, in the future, genetic nurse practitioners, Maher said.
Over time, research in the Division of Medical Genetics and Precision Medicine will expand beyond cancer, which is the focus now, he said. “And, increasingly, the division’s work will integrate with our colleagues in pediatric genetics.”
Maher’s research has already embraced the Jackson Heart Study – information obtained from studying about 5,000 African American men for decades. It holds a “wealth of data” that could help predict who is at risk for early heart disease, for instance, Ruckdeschel said.
For Butler’s part, he said he is “proud” of the new division in his department. “Not many places have someone with Dr. Maher’s expertise,” Butler said. “He is formally trained in both medical genetics and internal medicine. He’s a triple threat – in research, the clinic and education. He’s certified nationally, and his research on genetics and sickle cell disease is funded by the NIH [National Institutes of Health].”
By developing this new division, UMMC “is a little ahead of the game,” Butler said. “I believe we’re leading the way.”


