UMMC Department of OB-GYN delivers hope for 70 years
Editor’s Note: To commemorate the University of Mississippi Medical Center’s 70th anniversary, we will feature a series of stories throughout the year on the original School of Medicine departments established in 1955.
When Haylee Ladner learned she was carrying five babies, she was overwhelmed. She felt out of her depth, searching for a physician with the experience and confidence to take on what had suddenly become a complex pregnancy.
The months ahead felt uncertain and impossible to plan for—until a call from Dr. Rachael Morris, associate professor of obstetrics and gynecology and maternal-fetal medicine specialist at University of Mississippi Medical Center, changed everything.
“Dr. Morris reached out to me and gave me so much hope,” Ladner said. “She assured me that I would bring home five healthy babies. From that point forward, there was a full plan put into motion.”
By 17 weeks, she was admitted to UMMC where her care team had already reserved a private room in anticipation of her arrival and an operating suite ready for any emergency, at any hour. Each of the quintuplets was assigned their own NICU nurse, as well as their own neonatologists, all of whom had been on call in rotation as the big day approached.

“They were fully prepared for anything that could happen and took such good care of me and my babies,” she said. “I don’t think I could have possibly gotten better care at any other hospital. I’m so grateful to everyone on that team.”
The confidence and coordination that guided her care are the products of decades of progress—of the systems built, refined and reimagined to meet the needs of Mississippi mothers and infants. From its earliest days, the UMMC Department of Obstetrics and Gynecology has pioneered the consistent, collaborative approach to women’s health that continues to define the field today.
When the Medical Center opened its doors in 1955, the state was in the midst of a maternal and infant health crisis.
The state’s maternal mortality rate was more than 100 deaths per 100,000 live births, nearly double the national average at the time. Infant mortality was around 35 per 1,000 births, meaning one out of every 30 Mississippi babies did not survive their first year of life.
For thousands of women, especially those living in rural counties, the nearest hospital with obstetric care could be an hour or more away. Segregation and poverty compounded the barriers to access.
Dr. Michael Newton founded the UMMC Department of Obstetrics and Gynecology that same year. It was one small department in a brand-new medical center, but one that would become a lifeline for mothers and infants across the state. Over the next seven decades, the department’s journey mirrored Mississippi’s own, fighting one of the nation’s highest rates of maternal and infant death to achieving hard-fought progress driven by research, outreach and compassion.
In its first year, UMMC’s physicians delivered about 640 babies, frequently filling every available bed. Within five years, deliveries had doubled, and the budding department had added specialized clinics for infertility, cancer and high-risk pregnancies.
Newton understood that simply treating patients who made it to Jackson was not enough. Most maternal deaths happened far from the hospital in small towns, on farms and in homes without running water or prenatal care. Most of the deaths occurred among poor, rural Black women, many due to hemorrhage, infection or eclampsia that could have been prevented with timely medical attention.
When Dr. Henry Thiede succeeded Newton as chair in 1967, he brought with him an idea that was revolutionary for its time: that physicians and midwives could work together to reach women where they lived. Thiede believed that improving maternal outcomes meant expanding the health care workforce and decentralizing care.
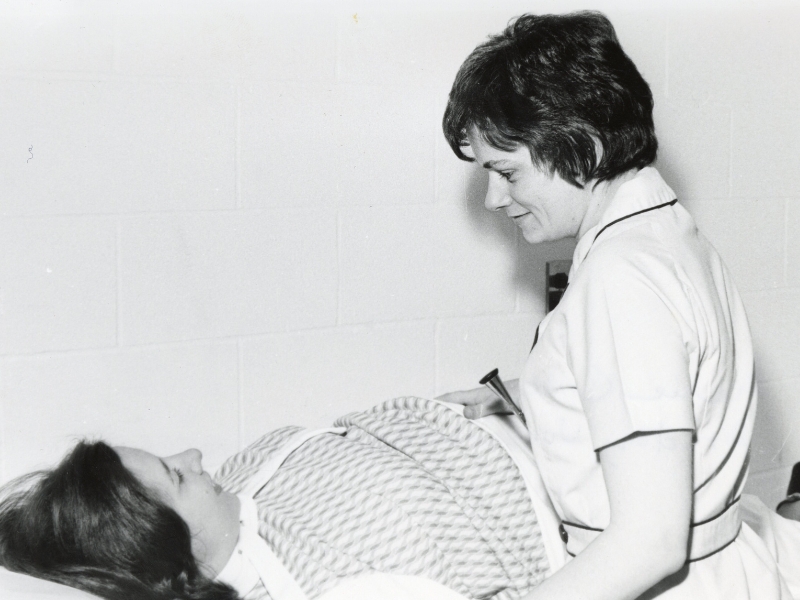
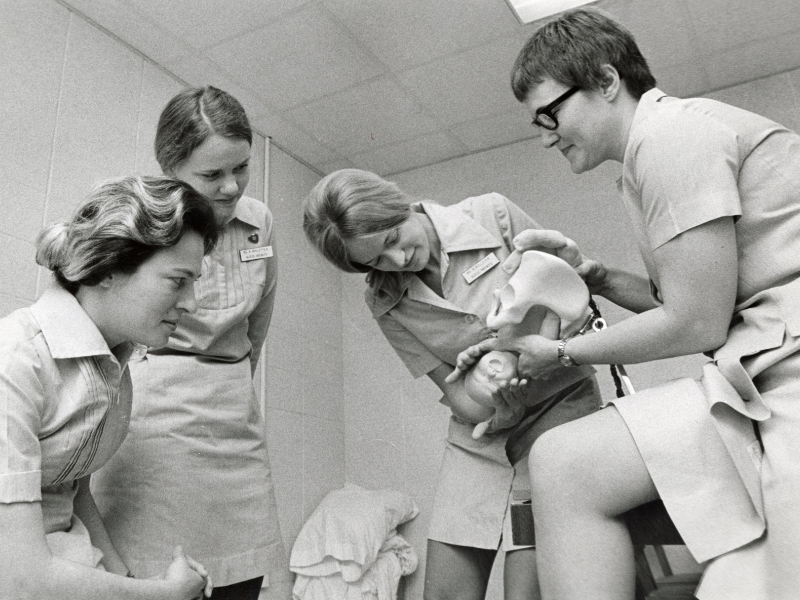
Under his leadership, UMMC collaborated with several state and national organizations to launch a series of initiatives supporting maternal and infant care. Staffing the department with nurse-midwives, the Medical Center was able to extend skilled care into rural communities. Midwives and physicians traveled to health departments weekly to provide prenatal, postpartum, family planning and OB-GYN care.
Through the creation of the County Health Improvement Plan, a partnership with the Mississippi Department of Health, the Medical Center designed the blueprint for nurse-midwifery education and integration into hospital-based care.
Midwives educated in Jackson staffed clinics in the Delta and Holmes County, creating a lifeline for families who otherwise had none. The infant mortality rate in Holmes County dropped from 39.1 deaths per 1,000 live births in 1969 to 18.6 in 1972, taking Mississippi from double the national average to just below it.
By 1972, UMMC’s nurse-midwifery program had become nationally acclaimed, hosting representatives from more than 40 states and several countries across Mississippi. It became the model for similar programs at institutions such as Emory University and the University of Pennsylvania, proving that collaborative, community-based maternity care could save lives.
By the time Dr. Winfred L. Wiser took over in 1975, Mississippi’s maternal and infant outcomes had improved significantly—and UMMC had established itself as the state’s epicenter for women’s health innovation.
When Wiser became chair in 1975, he inherited a department with only five full-time faculty, half the residency slots filled and no money for research. The annual budget was just $248,000. One of his first acts as chair was to establish a departmental research endowment, signaling to prospective faculty and residents that, despite the lack of federal funding available, research would remain a priority.
He recruited new specialists in maternal-fetal medicine, reproductive endocrinology and gynecologic oncology, tripling the faculty over his tenure. By the late 1980s, the department’s budget had increased tenfold, and its residency was attracting more than 200 applicants per year for six available slots.
In 1984, the department celebrated another milestone with the launch of Mississippi’s first in vitro fertilization program, one of the earliest in the nation. It was led by Dr. Bryan Cowan, who went on to chair the department from 2002 until 2009.
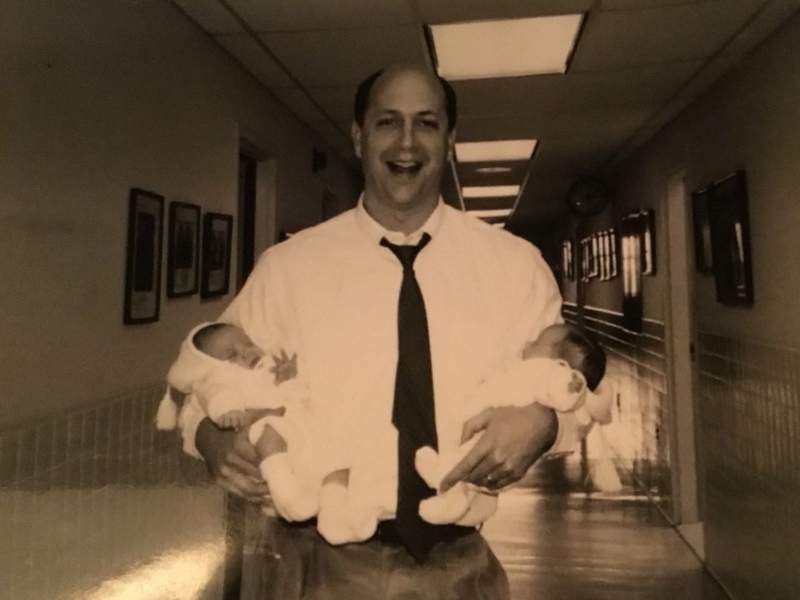
The IVF program gave new hope to couples who had exhausted every other path to parenthood, and, in 2024, it marked its 40th anniversary. In four decades, the program has helped hundreds of families welcome children who might never have been born otherwise.
“Since the introduction of IVF to UMMC, techniques such as direct sperm injection into eggs, as well as egg and embryo freezing have given couples better chances for establishing a family,” said Dr. Victoria Sopelak, former laboratory director of the IVF program. “It has also opened the door for patients seeking fertility preservation, especially those that have been diagnosed with cancer.”
But as the department grew, so did the demand. In the 1980s, UMMC physicians were delivering nearly 5,000 babies a year in facilities designed for half that number. Seventy percent of those pregnancies were considered “high-risk.” Delivery rooms overflowed into hallways, and obstetric emergencies often competed for space with routine births.
Amid growing demand and limited space, Wiser persevered, laying the groundwork for what he envisioned as a comprehensive perinatal center—a place that could bring obstetric, neonatal, and surgical expertise under one roof. His plans would take decades to realize but would ultimately reshape women’s health care in Mississippi.
The culmination of that vision came in 1999 with the opening of the Medical Center’s perinatal facility named for Wiser, honoring his decades of leadership and his contributions to women’s health in the state.
The first of its kind in Mississippi, the now-eight-story facility includes a mother-baby unit, surgical suites, lactation rooms and the only Level IV neonatal intensive care and OB-GYN emergency units in the state.
Under Dr. John Morrison, chair from 1995 to 2002, and Dr. James N. Martin Jr., director of the Division of Maternal-Fetal Medicine from 1991 to 2015, the department reached new heights of national and international recognition. Both men served as presidents of the International Society for Maternal-Fetal Medicine, making UMMC one of the only U.S. institutions to produce two leaders of that organization.
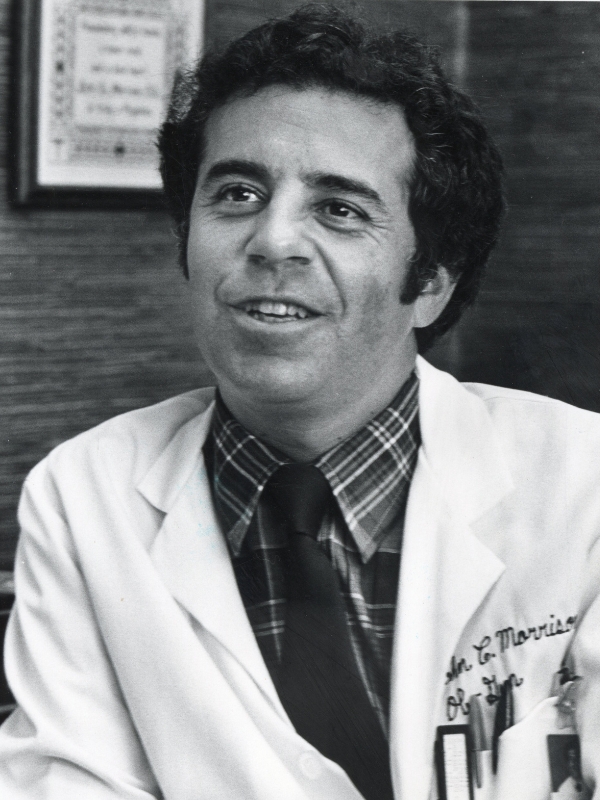
Under Morrison, the department strengthened its standing as a national leader in maternal-fetal medicine as he advanced clinical research and helped shape Mississippi’s modern perinatal system. Morrison developed and refined safer delivery methods for women with complex pregnancies—those complicated by diabetes, preterm labor, sickle cell disease, and hypertension—and secured a certificate of need to establish a statewide perinatal center, forming the cornerstone of regionalized perinatal care.
Widely regarded by ACOG as a global authority on hypertensive diseases of pregnancy, Martin’s work on preeclampsia and HELLP syndrome has saved countless lives. He is among the few physicians to have presided over all three major governing bodies in his field: the North American Society for the Study of Hypertension in Pregnancy, the Society for Maternal-Fetal Medicine, and the American College of Obstetricians and Gynecologists. As ACOG president, he championed global women’s health and gender equity and later joined the Preeclampsia Foundation’s national task force to develop landmark U.S. guidelines introducing patient education on early warning signs.
Despite 70 years of progress, Mississippi continues to face one of the highest infant mortality rates in the nation with nearly 10 deaths for every 1,000 live births. It also remains one of the states with the highest maternal mortality rates at 39.1 deaths per 100,000 live births in 2024. Cardiovascular conditions and hypertensive disorders remain leading causes, along with chronic illness, lack of prenatal care and postpartum follow-up gaps.
The department has continued to lead efforts to address the ongoing crisis. In 2014, UMMC joined the Mississippi State Department of Health to create the Mississippi Perinatal Quality Collaborative, aligning hospitals in the state around data-driven quality improvement. The first initiatives targeted severe hypertension and the “Golden Hour” of neonatal care, ensuring premature infants receive optimal support in their first 60 minutes of life.
Now, under Dr. J. Martin Tucker, Winfred L. Wiser Chair in Obstetrics and Gynecology, the department is expanding its reach once again. A five-year plan is underway to reintegrate certified nurse-midwives into UMMC’s hospitals and clinics. With a return to its roots, the goal is to offer round-the-clock midwifery coverage by 2027.

“The Department of OB-GYN is listening to the evidence,” said Janice Scaggs, a certified nurse-midwife at UMMC. “Research has shown good outcomes among individual low-risk women who receive perinatal care from midwives. When midwifery care is integrated into a health care system, unnecessary interventions are decreased, improving overall outcomes and reducing overall cost of care. Integrated midwifery care in the U.S. increases spontaneous vaginal delivery rates, lowers cesarean birth rates, increases successful vaginal birth after cesarean rates, decreases episiotomy rates, lowers preterm birth rates and low birth weight infants and increases breastfeeding rates-- all of which improve maternal and neonatal outcomes while supporting cost containment.
“Lowering unnecessary cesarean births will significantly decrease severe maternal morbidity and mortality associated with the overuse of cesarean birth. Bringing nurse-midwives and the midwifery model of care back to UMMC in a collaborative model with physicians is part of a vital solution to the challenges of providing high-quality, accessible care for all women and neonates in Mississippi.”

Tucker has also emphasized collaboration and education, expanding telehealth outreach, growing the OB-GYN residency program, and strengthening partnerships with the Mississippi State Department of Health to combat maternal mortality and morbidity through prevention, research and community training.
“I started my residency here in 1984 and have basically been with the Department of OB-GYN in some form or fashion for over 40 years now—45 if you include medical school,” said Tucker. “It's a privilege to be a part of its history and to have the honor of now leading the department.”


