Breathe easier over one less barrier to lung cancer screening

When Sammie Bass began having respiratory problems in spring 2020, he wondered if years of working at a brick manufacturer and inhaling dust on the job was the culprit.
“I got so that I could hardly breathe,” he said. “I got tired real quickly.”
After a March visit to the University of Mississippi Medical Center’s Flowood Family Medicine Clinic, the Jackson resident was referred to UMMC’s Cancer Center and Research Institute and the lung cancer early detection program because of his smoking history and age. Providers in the program recommended Bass be screened using a low-dose CT scan.
Dr. Michal Senitko, assistant professor of medicine and surgery and section chief of interventional pulmonology, and his team reviewed Bass’ scan. They went to work, rooting out the source of Bass’ discomfort as his breathing problems worsened.
The scan showed a mass rising from the lower part of Bass’ left lung, blocking his main breathing pipes. Senitko performed a bronchoscopy, an outpatient procedure under general anesthesia that allows a physician to examine a patient’s lungs and air passages. A small scope with a camera, with or without an ultrasound on the end, is inserted into the patient’s windpipe, giving the physician a view of tissues in the area.

Not only did Bass have a blockage, but the exam and a biopsy confirmed early-stage lung cancer. Senitko, as part of the same elective procedure, used endobronchial ultrasound to examine and biopsy Bass’ lymph nodes, which normally sit along a person’s main windpipe.
Senitko removed the blockage during the June outpatient procedure, allowing Bass to regain the use of the blocked parts of his left lung. Since then, Bass has been preparing for either chemotherapy, radiation, surgery or a combination, depending on his pulmonary function.
“I could breathe 100 percent better” after the bronchoscopy and removal of the blockage, Bass said.
Many Mississippians with risk factors for lung cancer need the screening Bass received, but until recently, Medicaid recipients had to pay for it out of pocket. That $150 cost was a roadblock for those on fixed incomes or with limited finances, said Jonathan Hontzas, a thoracic oncology nurse practitioner who with Senitko directs the Medical Center’s early lung cancer detection program.
However, the Division of Medicaid recently has begun covering the screening for patients who meet routine qualifications, such as being a pack-a-day smoker for 30 years, or two packs a day for 15 years. Bass, a retiree and past heavy smoker, is covered by Medicaid.
“This opens up the door for a whole lot of Mississippians who have Medicaid as their health insurance,” Hontzas said. “Giving Medicaid patients the same opportunity as others is a big deal.
“We’ve screened a lot more Medicaid patients in the last few months,” he said.
UMMC’s lung cancer early detection program is one of the GO2 Foundation for Lung Cancer’s Centers of Excellence. In addition to traditional bronchoscopy UMMC specialists perform electromagnetic navigation bronchoscopy. It uses 3-D imaging, GPS-like technology and a small flexible catheter to examine the lungs and take tissue samples.
That screening saves lives. Patients whose cancer is discovered in the late stages have a five-year survival rate of about 5 percent, Hontzas said. “You don’t have symptoms until the later stages, so outcomes are not good.”
But for those whose cancer is discovered early, the cure rate is as high as 90 percent. With screening, “we can decrease mortality by about 40 percent,” Hontzas said.
“Our goal is to catch them early enough that the patient can have a curative treatment,” Senitko said. “Most patients who present at the doctor’s office or an ER with a complaint related to lung cancer are in a later stage.”
When Bass was screened for lung cancer, Senitko said, “we found his cancer had progressed to the point where he had an obstruction.” To minimize wear and tear on patients, Senitko can perform multiple procedures at once. He takes into consideration the location of nodules or masses and other patient characteristics in devising the right strategy for each patient.
“The result is that the patient gets their diagnosis and cancer staging at the same time,” Senitko said.
“If we discover cancer, we talk about it at our tumor conference,” Hontzas said.
During that meeting, a group of doctors that can include pathologists, surgeons and medical and radiation oncologists discuss a patient’s case and come up with a plan for treatment. Surgery for lung cancer at UMMC is performed by specialists in the Department of Surgery’s Division of Thoracic Surgery led by Dr. Pierre DeDelva.
In Bass’ case, his pulmonary function isn’t optimal, making him more likely a candidate for chemotherapy or radiation. “He’s right on the edge of being a surgical candidate,” Senitko said. “We may start with chemotherapy, and then re-assess.”

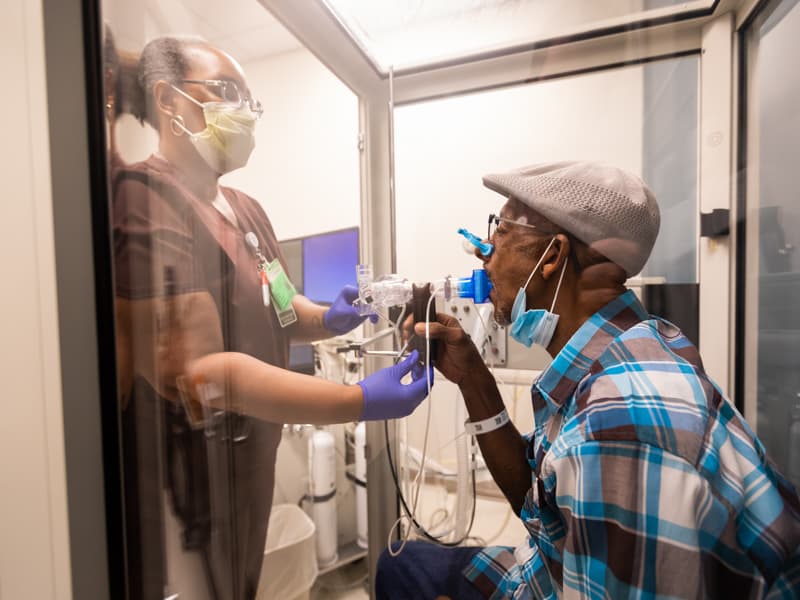
Bass recently underwent pulmonary function testing, which involved breathing in and out into a tube and riding a stationary bicycle. Pulmonary respiratory therapist Kimberly Lockett led Bass through breathing exercises as he sat in an open booth.
“Do you have any shortness of breath? What about a cough? What about smoking?” she asked.
Bass reported both shortness of breath and that he is a former smoker.
Lockett instructed Bass to blow into a tube – fast – as she waved her arm up and down so that he could match that frequency in blowing. “Keep blowing. Keep blowing. You’re almost there,” she encouraged.
“I’ll let you catch your breath. Take your time,” Lockett told him after he blew out air for a couple of minutes. After another round, they switched to Bass sucking in air.
“Suck it in deep! You’re almost there!’ she told him. “You have to follow my hand. In, out, in, out. Let’s go faster and deeper. I know it’s hard to do.”
“If more people get the screening you got, we can find more cancer that we can potentially treat and cure,” Senitko told Bass. “Sometimes, we do jobs in life that affect our health. We’re trying to help you long term.”
The role primary care physicians play in referring patients for screening is invaluable, Senitko said. “Nationwide, we screen marginal numbers of eligible patients, despite its proven mortality benefit. We believe that with the help of those standing on the front line and those providing primary care, we can save more lives.”
As he waits for additional treatment, Bass is optimistic about his recovery. “I’m trying to take care of myself,” he said.
It’s critical that Mississippi Medicaid recipients who qualify for lung cancer screening know that it’s now covered, Senitko said. “This benefit helped Mr. Bass,” he said.
“In his case, he might have shown up in the ED two or three months down the road because of the obstruction in his windpipe. He might have been diagnosed in a much later stage.”
For information about UMMC lung cancer screening and diagnostic tests, or to make an appointment, call (601) 984-5864.


