MSU interns work with mentors to design biomedical solutions
Four Mississippi State University biomedical engineering seniors have been working alongside University of Mississippi Medical Center faculty mentors this summer to identify a clinical problem and develop an innovative design to solve it.
The UMMC MSU Engineering Excellence in Device Development (UMEEDD) internship program, in its first year, matches students with researchers who have specific expertise in clinical sciences, basic biological sciences or applied engineering technologies.
When the summer leg of the 12-month internship ends later this month, it will be the beginning of Phase II for students, who then return to MSU where, enrolled in a senior design course, they will continue working on their project and meeting with mentors until April.
In the last phase, they will work toward goals that may include publication and an intellectual property agreement.
Maggie Phillips, from Decatur, Alabama, said the program is giving her the space to practice what she’s learned at MSU.
“We've gotten the opportunity to observe and study real-world problems people experience in health care and think about attainable solutions,” said Phillips, who plans on attending medical school after graduating next year. “As a pre-med student with an engineering background, my goal has been to use my training to make medical care accessible to those who need it.”

The School of Graduate Studies in the Health Sciences has a long-standing relationship with MSU’s Bagley College of Engineering, said Dr. Hanna Broome, associate dean and chair of the UMEEDD Advisory Board. Five years ago, they started brainstorming ways to collaborate, and the result was UMEEDD, which is funded by the Hearin Foundation through 2028.
“We hope this experience leads to the development of more Mississippi-based jobs and industries that are related to medical innovation through biomedical engineering-driven device and/or process development,” said Broome.
The internship has been enlightening and challenging, said Austen Breland, of Ellisville, who said he applied because biomedical engineers should have a thorough understanding of how the devices they design are used to treat patients.
“UMEEDD has provided me with valuable clinical experience and allowed me to get a better understanding of how to define problems from an engineering, clinical and patient-oriented perspective to arrive at the best possible solution,” said Breland.
Post-graduation, the mathematics minor wants to work in an engineering design or research role in the medical device industry, specifically with orthopedic implants. “While I have been faced with many questions I did not immediately know the answer to, my mentors have helped provide the tools I needed to independently seek out those answers.”
One of those mentors is Dr. John Clemmer, assistant professor in the Department of Physiology, who graduated from the same program at MSU – biomedical engineering – 15 years ago.

“I know how much of an impact the course had on me and my education at State,” said Clemmer. “We were limited to doing a senior design project using the resources at MSU, whereas the UMEEDD students have access to larger facilities, more faculty and a different/clinical environment.”
The interns were put in situations similar to what they will encounter in graduate school or academia, filled with challenges that force them to think outside the box, said Clemmer.
“It requires a lot of thinking on your feet, researching new areas in a short amount of time and persistent communication with possible collaborations. I have enjoyed seeing how they overcome obstacles and look for help and advice from different faculty when something doesn’t work or if it’s taking too long, which is very relevant for careers in medical research.”
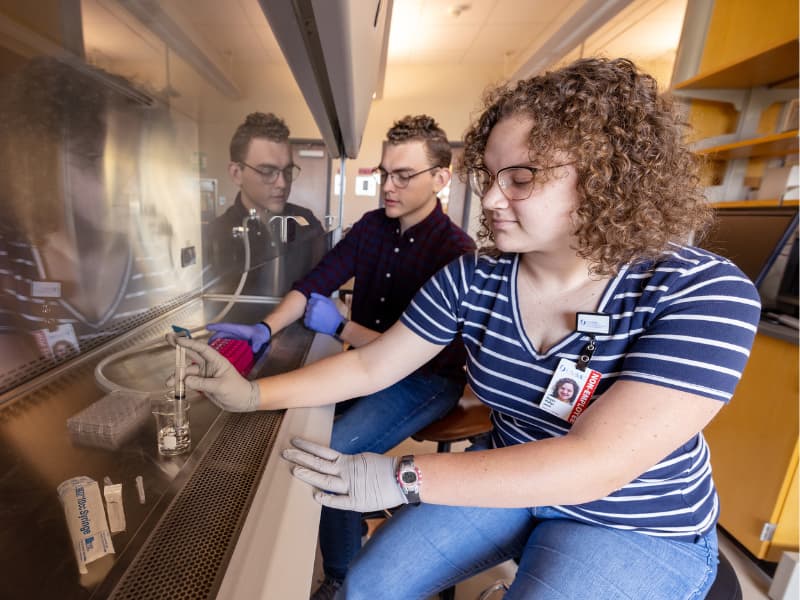
Mary Echelberry, who wants to go into prosthetic development after graduate school, said that after talking with their lead mentor, Dr. Matthew Kutcher, associate professor of surgery-trauma, the group decided to tackle chest tube removal. It’s a problem because when a lung is punctured through a traumatic injury, there is no quantifiable way of knowing if air is leaking into the chest cavity instead of expanding the lung, causing its collapse, known as pneumothorax.
“Because of this, it is hard to know if the air leak that caused the pneumothorax is properly healed to the point that a chest tube is no longer required,” said Echelberry, of D’Iberville.
With no way of determining if the lung has healed, physicians rely on trial-and-error, removing the chest tube to monitor the patient, and if the lung re-collapses, putting it back in and trying again in a few days, explained Joseph Rueff, of Madison, who wants to attend medical school.
“We are looking for a way to know definitively when one can take out a chest tube,” said Rueff. “Eliminating the need to replace a chest tube would reduce the length of stay of the patient and prevent discomfort.”
Over the next nine months, the four will work on building a model to solve that problem. After testing designs, they will present a final product at the end of their senior year.
The mentors have exceeded their mentees’ expectations, said Phillips.
“I have been astounded by the enthusiasm of the faculty here at UMMC to help us reach our goals,” said Phillips. “Every faculty member we have met has been quick to patiently answer our questions, provide resources for our study and open opportunities for us to explore both the center clinical problem and our personal interests beyond the project.”


