Gene therapy offers hope for sickle cell patients
Derrick James marched and played in band camp this past summer, and Kennedi Jackson dances.
The two Mississippi teenagers – 16 and 13 respectively – are enjoying their favorite activities without the sickle cell disease pain crises that they endured since early childhood. Derrick, DJay to friends and family, and Kennedi were among the youngest patients in clinical trials for new gene therapies targeting sickle cell disease.
On Dec. 8, the FDA approved Casgevy and Lyfgenia, the first cell-based gene therapies for the treatment of sickle cell disease in patients 12 years and older.
Children’s of Mississippi, the pediatric arm of the University of Mississippi Medical Center, is home to the Center for Cancer and Blood Disorders and one of the nation’s largest pediatric sickle cell disease programs. UMMC will be a clinical trial site for gene therapy for sickle cell disease later this year.
DJay’s fortune
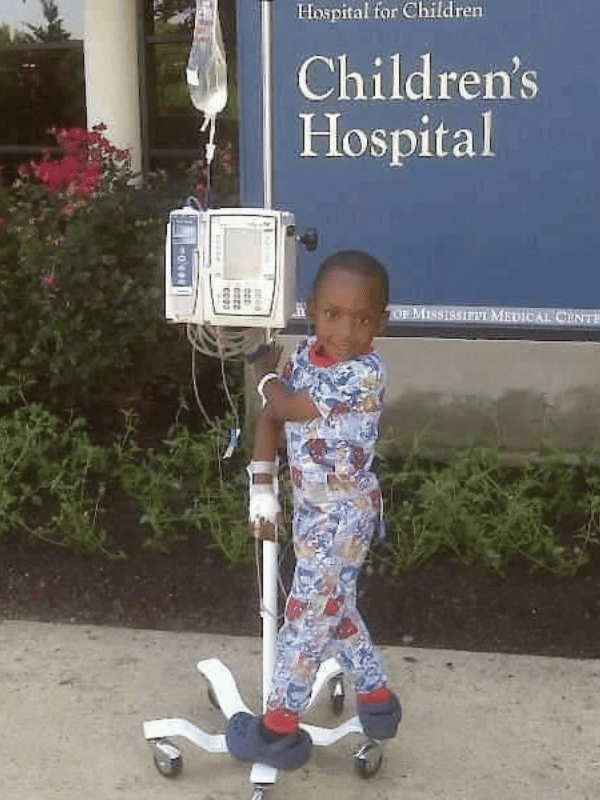
DJay, a patient of Dr. Dereck Davis, associate professor of pediatric hematology and oncology, was struggling in 2019.
“There were a lot of pain crises and a lot of missed school,” said his mother, Lashaunda Kincaid of Raymond. “D’Jay required monthly blood transfusions and numerous admissions. Every fall we knew DJay would be admitted at least 2-3 times. In 2019, things had become difficult.”
Healthy red blood cells are round and carry oxygen throughout the body. In a person with sickle cell disease, those cells are shaped like a sickle and become hard and sticky. Those sickle cells die early, causing a shortage of hemoglobin, and they clog the blood flow in small blood vessels. This can cause pain and complications such as stroke, infections and acute chest syndrome, a pneumonia-like illness.
Bone marrow transplant has been the only known cure for sickle cell disease. The procedure replaces abnormal stem cells with healthy cells from a matching donor. DJay did not have a close enough match, making a clinical trial for Lyfgenia at Children’s Hospital of Atlanta a lifeline.
Lyfgenia, a cell-based gene therapy developed by Bluebird Bio, genetically modifies a patient’s blood stem cells to produce a therapy-derived hemoglobin that functions similarly to the hemoglobin produced by a person who does not have sickle cell disease. Those modified stem cells are then returned to the patient through an infusion.
“We knew we needed to do something,” Kincaid said, “but it was uncharted territory, so it was scary.”
The decision to try gene therapy wasn’t easy, she said, and there was extensive testing that was done prior to approval. “For nearly a year we traveled back and forth to Atlanta for consultations, discussed the risks with Dr. Davis, and prayed intensely.”
A fortune cookie at P.F. Chang’s gave the family a sign. “It read, ‘You will enjoy good health; that is your form of wealth,’” she said.
The process wasn’t quick or easy. After a year of trips to Atlanta for testing, DJay was in Atlanta undergoing chemotherapy to prepare for the Lyfgenia dose. He was 13 at the time.
Though the COVID-19 pandemic had started, Kincaid said the strict infection control measures involved in bone marrow transplant and the clinical trial meant that DJay was well-protected from viruses.
When DJay received his dose of Lyfgenia, “we did a Zoom call with Dr. Davis and the Mississippi Sickle Cell Foundation so we could all be connected.”
Kincaid said the risks of the treatment were worth it. “I tell people, yes, there are risks, but if you have sickle cell, every day is a risk. Dr. Davis was with us every step of the way. Our family’s faith in God carried us through the process.”
By mid-September 2020, DJay was home. Once homeschooled because of frequent pain crises, he is now a junior at Raymond High, where he plays trombone in the band, and enjoys fast-paced basketball games with friends after school.
“He even went to this past summer’s Baby Boom band camp at Jackson State University,” Kincaid said. “He was able to make it through and had the same energy level as the other students.”

In December, DJay went snow tubing. Since wintry weather can trigger a pain crisis, a Christmas trip to the slopes wasn’t something he could enjoy before his infusion.
“Our family truly appreciates Dr. Davis and our support system,” Kincaid said. “They and friends, family and faith saw us through.”
With an eye toward a music degree from JSU, DJay said he’s been “catching up” since his gene therapy treatment, doing the things that he once couldn’t do easily.
“Now I can hang out with my friends,” he said. “It’s a completely different life.”
Kennedi’s Christmas
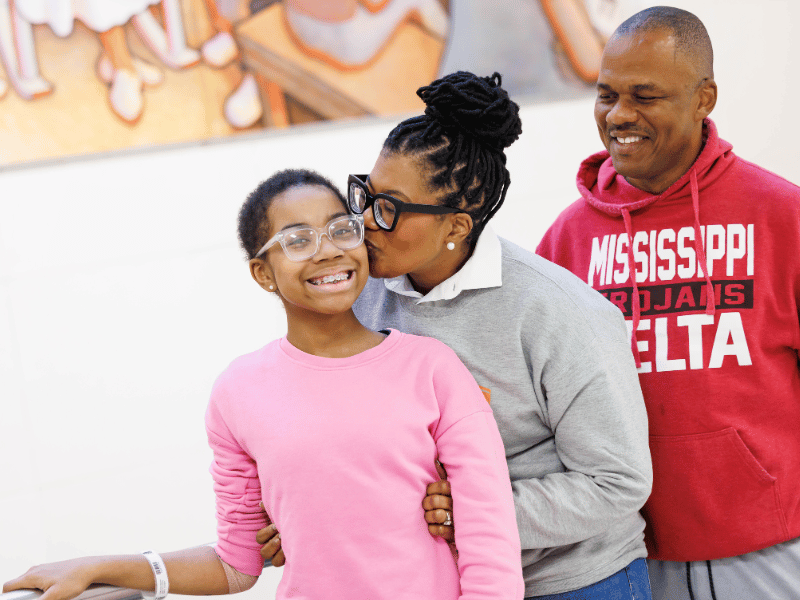
This holiday season was different for Kennedi Jackson – she was pain free.
The 13-year-old eighth-grader hasn’t had a pain crisis since May 1, 2023, the day she became one of the youngest sickle cell patients to receive an infusion of her own stem cells.
“Since then, one of the biggest things we’ve had to learn since then is how to be well,” said her mother, Kashanta Jackson of Moorhead. “For 13 years, she wasn’t.”
Since birth, Kennedi had averaged three to four hospital stays a year and was in “bone-crushing pain” multiple times a month, her mother said. A cold snap could easily send her into a pain crisis.
“I’d rather have the pain myself than for her to suffer,” said her father, Dr. Tyrone Jackson, president of Mississippi Delta Community College.
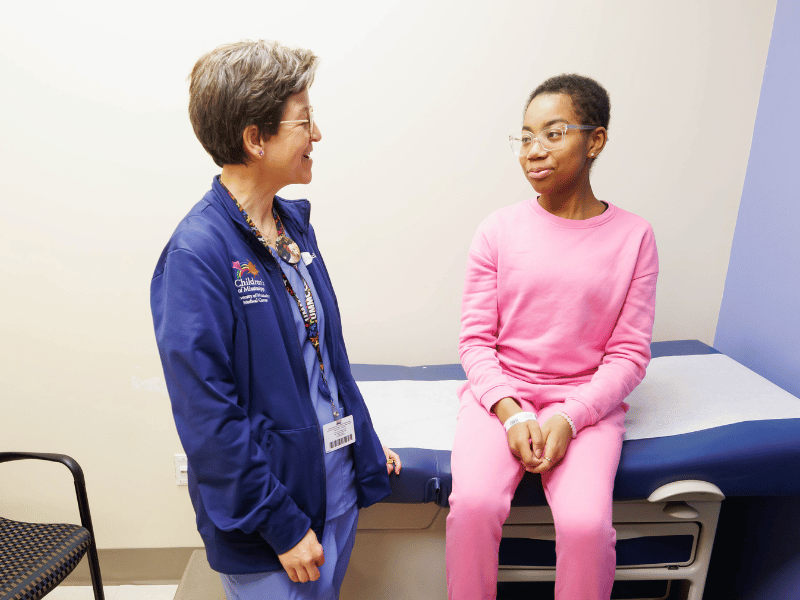
Kennedi, a patient of Dr. Melissa McNaull, professor of pediatric hematology and oncology, was being considered for a bone marrow transplant with her older brother as a donor. Instead, the doctors suggested a new treatment that was then the focus of a study at TriStar Centennial Medical Center in Nashville, Tennessee.
In her treatment, Casgevy, developed by Vertex Pharmaceuticals and CRISPR Therapeutics, CRISPR is used to edit blood stem cells to increase the production of fetal hemoglobin. Just as in the womb, increased levels of fetal hemoglobin prevent red blood cells from becoming sickle shaped.
For her treatment in the clinical trial, Kennedi was admitted to TriStar Centennial, where she stayed for about three weeks prior to her infusion and for several weeks after.
“We knew I-40 well,” Tyrone said. “We were taking turns staying with her.”
When the time came for Kennedi to receive the infusion, “it came in a huge freezer,” Kashanta said, “but what they took out was a little tube.”
The little tube made an enormous difference. “Kennedi is now functionally cured,” McNaull said.
Undergoing treatment “was scary,” Kennedi said, “but my parents were there for me, and that made it easier.”
Post treatment, Kennedi sees doctors at TriStar Centennial every three months and her physicians at Children’s of Mississippi every two months.
“We are so appreciative of Kennedi’s entire medical team,” her father said. “They have gone above and beyond for her and our whole family. We can’t thank them enough.”
Before gene therapy, chronic pain was a constant for Kennedi. “Many, many emergency room visits and hospital stays,” her mother said. “Sickle cell has been a constant in her life, but it’s been unpredictable. She could be fine one minute and facing a life-threatening emergency the next.”
Today, Kennedi isn’t missing school at Indianola Academy for sickle cell emergency care, and Kennedi is enjoying jazz, hip-hop and ballet dancing as well as cheerleading.
Kennedi’s medical journey brought her health today and inspiration for tomorrow. “I want to be a nurse one day,” she said, “and treat children with sickle cell.”
Hope for a cure
Davis said the two new therapies offer a chance for a healthier life to a population in need of alternatives to bone marrow transplant.
“This is offering hope to a population of patients and their families who have been starving for good options,” Davis said. “These therapies are not without risk, but they have been shown to work. The challenge will be in access to this care.”
Prior to treatment, a patient must undergo high doses of chemotherapy, which removes cells from the bone marrow so they can be replaced with the modified cells in Casgevy and Lyfgenia.
While these therapies offer hope to sickle cell patients, there are obstacles to care. Casgevy and Lyfgenia are best suited for sickle cell patients who do not have organ damage from the disease and are strong enough to undergo chemotherapy.
Another issue with these therapies is the price. “Both of these technologies are expensive,” Davis said. The price of Casgevy is $2.2 million for a single treatment, while the price of Lyfgenia is $3.1 million.
“The evidence shows that this works, and for the patients who need this, we’re so excited that this is available,” McNaull said. “Improvements will come in the future, so we think gene therapy will be different and better.”
The Mississippi Sickle Cell Foundation will host a Parent & Warrior Support Group meeting where Davis will discuss gene therapy options for sickle cell at 10 a.m. Jan. 27 in the Jackson Medical Mall Community Room. For more information, email mssicklecellfnd@yahoo.com.


