OpenNotes promotes transparency in medical records
You've just walked out of a clinic appointment with your UMMC physician. You wish you'd written down what the doctor explained as she typed up her notes and listened more closely to what your blood test results meant.
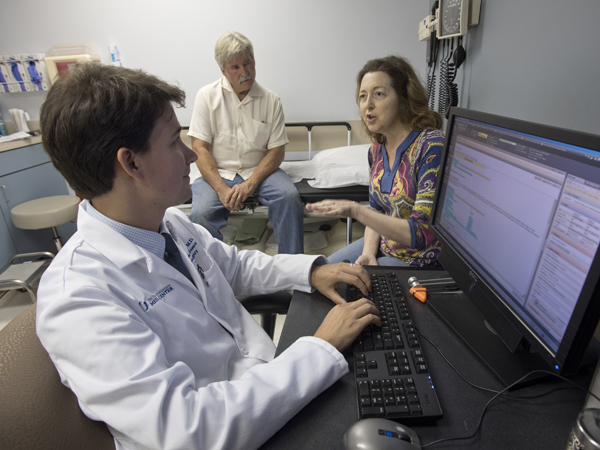
Patients can get quick and secure access to the notes their providers take during outpatient visits by using a form of communication advocated by a national nonprofit organization. It's called OpenNotes, an initiative that UMMC providers will take part in beginning Sunday, Jan. 8.
According to its creators, OpenNotes promotes transparency in medical records and empowers patients to not only monitor their care, but catch errors in caregivers' notes that could result in harm. It creates a new partnership between patients and their providers.
On its website, the OpenNotes organization estimates patients quickly forget up to 80 percent of the verbal information their caregivers provide to them.
“This helps the patient understand what they've been told in clinic,” said Dr. Louis Harkey, Robert R. Smith Chair of Neurosurgery, who's helping to spearhead the effort. “And this can have huge safety benefits if a patient finds an error.
"This creates a collaborative relationship between the patient and provider.”
“It's definitely a culture shift for us, that's for sure,” said Dr. Shannon Pittman, professor of family medicine and director of the Family Medicine Residency Program. “But it will create lots of opportunity to adopt the culture of 'The information in the record is the patient's information.'”
Physicians write chart notes to remind themselves about their thoughts at the time of the visits. They use notes to communicate with other physicians about their evaluations of patients and to document what thought processes they used and what decisions they made in case that activity is questioned later.
How does OpenNotes works? Notes typed during a visit are signed by the provider in a patient's secure electronic records section that can be accessed via a portal if the patient signs up for MyChart. Patients with MyChart can manage facets of their care electronically - from sending a message to their provider's office to reviewing test results and their health summary to scheduling appointments.
With OpenNotes, as soon as a provider's notes are signed, the patient will receive an email reporting the notes are ready for viewing in MyChart, Harkey said.
If a patient sees a mistake, he or she can indicate that in MyChart and request the error be corrected. Examples of good catches by patients could be hyperthyroidism listed instead of hypothyroidism, or “no malignancy” written as “now malignancy.” OpenNotes “automatically notifies (UMMC) Compliance” if a patient alerts a provider to an error, Harkey said.
A provider can opt out of making available a particular set of notes, but can't blanket opt out of OpenNotes, Harkey said. Only providers for limited, selected services - for example, adolescent medicine, or some aspects of mental health - can totally opt out because note information is often sensitive.
“Giving patients access not only to verbal communication of our thoughts, but access to a written record of that, is always a good thing,” said Dr. Mark Earl, associate professor of transplant surgery and director of the General Surgery Residency Program. “OpenNotes gives them the opportunity to go back, review and better understand what we talked about.
"All that can do is create a more educated and insightful patient.”
Not all UMMC physicians and providers are comfortable with OpenNotes, however. Some believe it will require them to write their notes differently, knowing that patients will be reading them. Another concern is that “some of the medical language and speculation in the chart note may be frightening to the patient or presented prematurely, and that would not be in the patient's interest,” said Dr. James Sones, professor and chief of the Division of Digestive Diseases.

Instead, Sones said a personal and more direct communication could be the better alternative when facts are known, “and in a manner that would be kinder.
“Is this 'keeping secrets' from the patient?" asked Sones, who does not oppose OpenNotes. “Perhaps a strict definition could interpret it that way, but the chart and its contents are available to the patient at any time, just not as the default, real-time choice.”
Dr. Robert Brodell, professor and chair of dermatology, is conflicted on OpenNotes - but said it's clear the vast majority of patients would like access to their own medical records.
“My knee-jerk reaction was fear,” Brodell said. “Patients might read my note and misunderstand something I'm writing. My notes are in medical-person language, not lay person language.
"I'll need to write notes more carefully so as not to offend a patient with my current note-writing language that is descriptive, but not sensitive to a patient's feelings.”

Brodell said he worries that information could get into the wrong hands if a patient's password is stolen, or if they fall prey to phishing.
“This is a double-edged sword,” he said, but “some patients undoubtedly will catch a mistake - a mislabeled location, or a lab not reported to them because we had trouble reaching them when a nurse was on vacation.”
Nationally, 11 million patients have access to OpenNotes, which sprang from a 2010 study involving more than 100 primary care doctors that explored how sharing notes impacts health care. OpenNotes is grant funded, and hospital systems taking part include the M.D. Anderson Cancer Center, the Ochsner Health System, the Penn State Hershey Medical Center and all Veterans Administration Medical Centers.
OpenNotes estimates that up to 92 percent of patients with access to their notes open them, and more than 70 percent have said it helps them feel more in control of their care.
Earl doesn't believe OpenNotes is an inconvenience for caregivers.
“There's not extra work to be done,” he said. “The medical records belong to the patient. Who do we work for? It's the patients.
“It's very plausible that an incorrect diagnosis could be documented in a chart and then just get carried forward. This adds another layer of security to ensure their medical records are accurate.”
At UMMC, OpenNotes won't be used for inpatients or for those coming through the Emergency Department who generally don't have an ongoing patient/provider relationship for that visit.
On its website, OpenNotes includes “do and don't” suggestions for writing notes. The “do” list includes explaining to patients what they might expect to see in notes, incorporating lab or study results, and focusing discussions on the situation at hand. Suggestions also include softening certain language, such as saying “patient could not recall” instead of the medical term “poor historian.”
The “don't” list cautions against oversimplifying notes, omitting important sensitive issues, using judgmental terms (such as fat or angry), and using jargon or abbreviations that are a mystery to some patients or can be misunderstood - for example, SOB instead of short of breath.
OpenNotes promotes transparency as opposed to the “cloak of medicine” that serves to shield notes from a patient, Pittman said.
“This forces us to think about it in a different way,” she said. “It's an opportunity to embrace an area where we haven't been before.
“The patient will know what I know. They will see my thought process. Even when we make a good effort to be a good communicator, sometimes, we're not.”


