COVID-19-burdened UMMC braces for tacked-on crises

Here’s a conversation starter: What if the world threw a pandemic and a second catastrophe crashed the party?
How will Mississippi find enough beds for a new flood of patients produced by another calamity to be named later – a flu outbreak or a natural disaster approaching that of Hurricane Katrina?
If beds are found, how will the state find enough health care workers to staff them, or equipment to protect them? And, if there aren’t enough beds or staff, who decides which patients are turned away?
Even now, during hurricane season, COVID-19 alone is doing a great job of tormenting the state with those very issues, and a flu outbreak lurks in the offing.
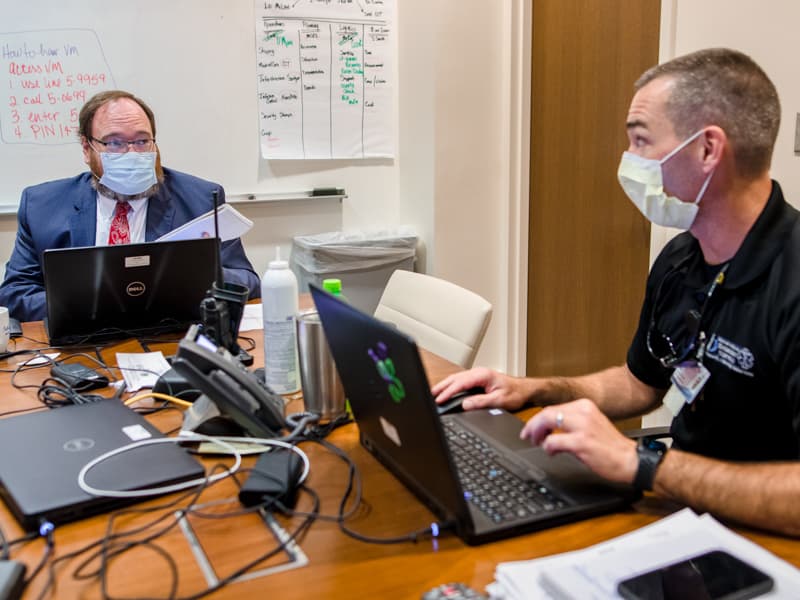
Whatever COVID-coinciding crisis may occur, one thing is certain: “No cavalry is coming over the hill to save us,” said Dr. Jonathan Wilson, chief administrative officer and COVID-19 incident manager at the University of Mississippi Medical Center.
Fortunately, many of those wearing the boots on the ground united recently to ponder double-disaster scenarios and make recommendations to the state’s hospitals.
Attending the video-conferenced “Tabletop Exercise” were representatives of UMMC; the Mississippi State Department of Health; other health care experts and coordinating bodies, including the Mississippi Emergency Management Agency.
They contemplated a complicating threat tacked onto what calls “the latest bogey man – and the latest is always the biggest,” said Terry McLeod, clinical director for the Mississippi Center for Emergency Services at UMMC. In Mississippi, this one sprang out of the closet four months ago, although it seems like four years.

Perhaps the last big bogey man, before now, was Hurricane Katrina, back when McLeod was a nurse manager at UMMC.
“Could we deal with a pandemic the same time as a hurricane?” McLeod said. “Absolutely. We have an extremely rich history of people who have been in the trenches; they know how to make decisions. But you can have all the decision-making in the world, you can come up with the perfect plan, if everybody doesn’t do their part, it’s not going to stick.”
Decision-makers have little control over people’s behavior in, among other places, hurricane shelters. With large numbers of storm victims and evacuees huddled in those shelters, you have “a recipe for helping this virus to spread,” Wilson said.
“The concern is there won’t be adequate social distancing. You would have to depend on people wearing masks. Shelters would have to operate at less than maximum capacity, which means opening more of them, and the American Red Cross would have to find people to staff them.”
It would be a challenge, McLeod said. “But, since Katrina, there’s a lot more experience under a lot more belts. We had good people with good, walking-around common sense doing the best they could in a bad situation, and we pulled it off.”
The Medical Center and Mississippi need that grit.

Just six days after the July 8 Tabletop session, the Medical Center’s leader told “World News Tonight”: “We are full.” The adult hospital was “oversubscribed,” with many more patients than beds, said Dr. LouAnn Woodward, vice chancellor for health affairs at UMMC.
That same day, Dr. Alan Jones told a Jackson news station: “Hospitals have a breaking point.

“We may not have a place to put a trauma patient,” said Jones, professor of emergency medicine and assistant vice chancellor for clinical affairs at UMMC.
“We may not have a place to put a sick heart attack patient or a stroke patient, because we have all these other patients that are in the hospital, and they need to be there.”
Finding more room depends, in part, on more people agreeing that an ever-rising number of COVID-racked hospitals and (as of this article’s publish date), the deaths of some 1,300 Mississippians aren’t the figment of someone’s agenda.
“It’s an everybody game,” Jim Craig, director of health protection at MSDH, said during the Tabletop session. “It’s not just the health department’s pandemic.”
Not everyone is playing by the games’ rules: mask-wearing, social distancing, hand-washing, kegger-shunning. In the meantime, said Dr. Thomas Dobbs, State Health Officer, addressing a July 9 news conference, Mississippi’s hospitals are left to contend with the “impacts of reckless social behavior.”
The penalties for that behavior will be multiplied should two or more resource-draining catastrophes intersect – something that has occurred in Mississippi before, more or less. Actually less, since not one of them is in COVID-19’s league.
For his part, Craig remembers two separate triple-terror episodes. The first: The 2009-2010 H1N1, or swine flu, pandemic, when MSDH also took on Tropical Storm Claudette and Hurricane Ida.
The second: The Zika virus epidemic a few years ago, which overlapped a deadly Hattiesburg tornado and “a flooding event.”
Years before those ordeals, immediately following the terrorist attacks of September 11, 2001, Medical Center and MDSH officials joined forces to prevent the state from getting caught with its beds down.

“We were concerned about the potential for a bioterrorism attack,” Wilson said. “9-11 was the starting point. But a lot of the bigger lessons we learned were during Katrina, and a lot of smaller ones during other disasters, such as the Mississippi River flood of 2011.”
While Katrina-induced levee failures terrorized New Orleans with flood waters 15 years ago, the Mississippi Gulf Coast and its many neighbors to the north suffered their share of heart break.
Soon after the August 29 storm, Wilson, who was an ER nursing supervisor at the time, joined an eight-person Medical Center crew dispatched to weigh the Coast’s emergency care needs; for several days, it provided them as well.
“We became a triage team. We had to improvise,” said Wilson, who splint a man’s ankle in Bay St. Louis with a two-by-four from a debris pile.
But UMMC was unable to spare a long-term relief team. This was no way to take care of patients, Wilson and his colleagues decided. What Mississippi needed, especially during times of mass casualties, was a way for hospitals and emergency responders to communicate better, a way to mobilize timely help and coveted resources wherever the need.
And that’s why the Mississippi Center for Emergency Services was born and, along with it, Mississippi MED-COM, a 24-hour communications center with headquarters at UMMC.
“A response to an emergency requires people working together, and a centralized view of the medical situation,” said Dr. Kendall McKenzie, professor and chair of emergency medicine at UMMC. “That’s what the state has now, and didn’t have during Katrina.”
By 2011, the state had another advantage it lacked six years earlier: FAST.
The Forward Assessment and Scene Triage team makes sure the right care and equipment gets to victims rocked by widespread disease, or, as the case was following the tornado outbreak of April 2014, widespread destruction – particularly in Louisville, where the ER at Winston County Medical Center flooded.
“This was a chance for the medical community to shine,” McKenzie said.
There, in Louisville, UMMC assembled an eight-bed hospital inside an 18-wheeler trailer. “Now, we have experience setting up mobile hospitals, which we didn’t with Katrina,” McKenzie said.
That same year, once the Ebola virus began killing its way from Africa toward the U.S., the Medical Center engineered a care unit with state resources. Ebola patients never materialized, but priceless know-how did.

“Learning what I learned from Ebola has really helped my ability to assist with COVID-19,” said Jason Smith, manager of emergency services at UMMC, who helped marshal the Ebola unit.
“You learn that you don’t want to bring that virus out of the room. You learn to adhere strictly to guidelines to protect the patient and yourself. We also had to dive deeper into PPE [Personal Protection Equipment], just as we have to do now.”
Each confrontation – Katrina, Louisville, Ebola and more – brought to bear what McLeod calls the Medical Center’s “greatest asset: our ability to solve problems, even if the problem had a different name last time, whether it was hurricane, tornado or pandemic,” he said.
But it’s been a while since anyone faced a plague on the scale of COVID-19. “No one has seen a pandemic this bad since the 1918 flu,” Wilson said.
Like the tides and taxes, the flu is inevitable. “It will be a major complication in the fall,” Craig said.

Asked what concerns him more, a flu outbreak or major hurricane vis-a-vis a pandemic, Stephen Houck said, “Honestly, you have to worry about all three.
“But hurricanes don’t worry me as much as the pandemic and the flu,” said Houck, director of the Mississippi Center for Emergency Services.
The folks at the Centers for Disease Control and Prevention were concerned enough about this exponential threat to develop a test that can check for influenza A, influenza B and COVID-19 at the same time.
Compared to the flu, as Houck pointed out, a hurricane’s clout, no matter how destructive, is limited. “With the flu, and COVID, those patients are everywhere,” he said. “And if people get sick in the tri-county area, they’re going to come to UMMC.
“But we’re working with the state health department to try and be more efficient about making sure patients, as long as they can be taken care of, don’t all come to only one hospital or to only a few.”
At any hospital, a flu outbreak can lay waste to nursing staffs, on top of decimations by COVID-19. If a hospital loses nurses, it also loses beds, Houck said. “Even with enough beds, you can’t fill them if you don’t have the staff.”
So, the question remains: When a hurricane, or the flu, drops in, what will have to give in this COVID world?
Bed sheets, for one thing. Patients may not get their bed sheets changed every day. It may sound like a small thing, but that’s one of several recommendations meant to give overwhelmed staffs a break. Those recommendations, proposed during the Tabletop exercise, included providing fewer bed baths.
Bed baths and linen changes occupy the territory known as Standard of Care, normal hospital practices that can be reshaped by abnormal times, such as a "catastrophic disaster."
That may mean doubling up patients in hospital rooms or placing them in hallways or the ER. It may mean securing beds or cots elsewhere. Or creating mobile hospitals – a version of M*A*S*H units in the war against Coronavirus.
Or making sure PPE goes first to hospitals and other care facilities with the greatest number of cases. Or housing an overflow of recovering patients in institutions prepared for them, including Camp Shelby in Hattiesburg and, in Fulton, Itawamba Community College.

“If hospitals are full,” Craig said, “we have contingency plans in place and, in some cases, contingency plans to the contingency plans for using alternate care sites.”
It may mean doing what no health care decision-maker does lightly: “decompressing” – discharging some severely ill patients to those nursing homes accepting high-acuity cases.
“Discharging them too early is a concern,” Wilson said, “especially considering the acuity of our patients at the Medical Center. How do you prioritize patients and do so consistently and ethically?”
Ideally, Craig said, every facility should have “an ethics committee to consider these questions.”
Whatever answers may come, solutions are at the mercy of the people they’re meant to help. “No amount of extra beds can compensate for the public’s disregard for social distancing and other measures,” Dobbs told his colleagues just days before announcing that the state’s 10 ICU’s were full.
As Smith put it: “We are doing everything we can do to make sure we are taking care of Mississippians, but Mississippians need to be prepared as well.”
It’s a matter of “personal responsibility,” McLeod said. “It takes every individual saying, ‘I’m going wear my mask, I’m going to wash my hands, I’m going to maintain social distancing, I’m going to get my hurricane preparedness plan together.
“This means you.”
When it comes to that, McKenzie clings to his memories of his post-Katrina experience in Mississippi, when his National Guard unit from Panama City recovered victims’ bodies in Bay St. Louis.
“It amazes me how much people step up to the plate here,” said McKenzie, who moved to Mississippi from Florida. “Having another disaster on top of a pandemic, clearly, will tax all systems, but the one thing that won’t go away is volunteerism.
“After Katrina came through, there were so many good-hearted people who came down, there wasn’t enough food and water or places to stay for everyone. They had to ask people to stop volunteering to help.”
No one will make that request this time.


