Patents, trademarks display UMMC’s innovation
At the end of the last fiscal year, the U.S. Patent and Trademark Office issued the University of Mississippi Medical Center two patents and a trademark. Combined with record numbers of intellectual property applications and disclosures, these inventions represent the diversity of approaches our faculty take to advancing science and health care.
The Bench
About one in ten people in the U.S. have some form of chronic kidney disease, which kills about 50,000 Americans yearly.
“Currently, there are no effective treatments to reverse the course of chronic kidney disease,” said Dr. Alejandro Chade, professor of physiology and biophysics.
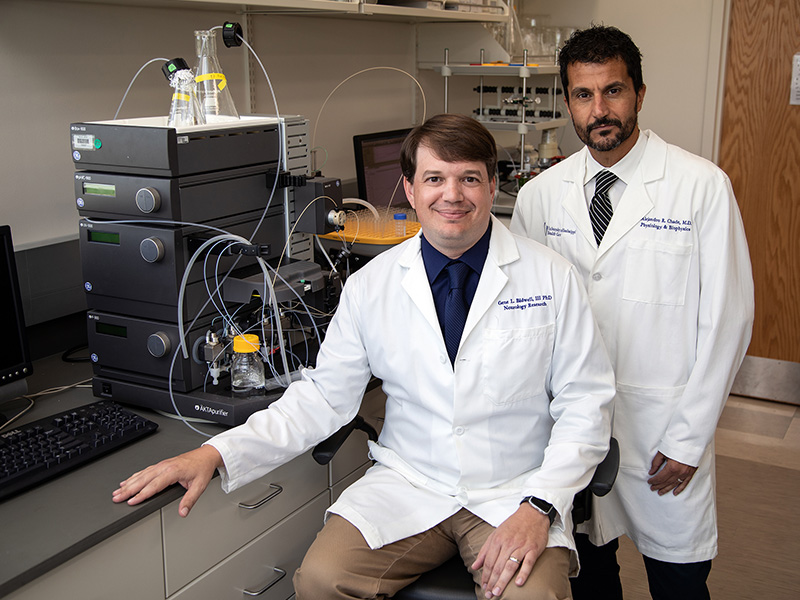
Chade is the co-inventor of a patent that covers the use of an elastin-like polypeptide, or ELP, to deliver drugs to the kidney. This patents also covers the use of a protein that promotes blood vessel growth in order to slow the progression of kidney disease. Chade, who studies vascular diseases, worked with co-inventor Dr. Gene Bidwell, associate professor of neurology, to create the drug delivery system.
“ELP naturally accumulates in the kidneys, so we take advantage of that characteristic by fusing therapeutics to the protein,” said Bidwell, who has worked with ELP for more than a decade.
This is the sixth patent UMMC has been issued for an ELP-based technology, which collectively are the foundation of UMMC’s drug delivery system ELP BiologicsTM. Like a molecular set of Lego-blocks, it can be built to hold different kinds of therapeutics and target organs.
In this newest iteration, the therapeutic is VEGF, or vascular endothelial growth factor. In advanced cases of CKD, VEGF production decreases.
“By giving VEGF back to the kidney, we can restore some of these blood vessels,” Chade said. In the pre-clinical models, “We see about a 40 percent recovery of kidney function, less fibrosis and more vessels.”
While not a cure, it represents a major advance towards treatment. Slowing the progression of kidney disease would mean lengthening the time a patient has before needing to pursue dialysis or a transplant.
Before Chade and Bidwell can move forward to human testing, they must do additional work testing for toxicity and efficacy beyond the four-week window post-infusion that they studied.
In the future, they plan to partner with a laboratory that meets the Food and Drug Administration’s Good Manufacturing Practices certification to produce their molecule at clinical quality suitable to for Investigational New Drug status.
The Bedside

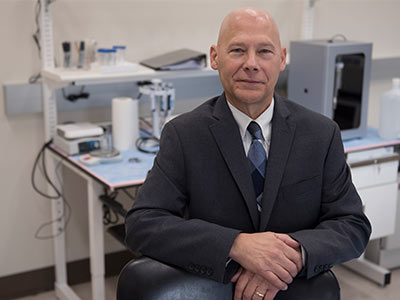
In late 2018, Dr. Alan Jones and colleagues published findings from a clinical trial testing carnitine as a way to treat sepsis.
“We found a subset of patients that responded to the carnitine treatment,” Jones said. “Through blood tests, we identified which patients had the bioenergetic mechanisms to handle this treatment,” said Jones, professor and chair of emergency medicine.
Those mechanisms, represented by smaller amounts of certain chemicals in the blood, formed the basis for a patent that covers those biomarkers and their diagnostic use in carnitine-based sepsis treatment.
Jones, professor and chair of emergency medicine, is one of the inventors, along with Dr. Michael Puskarich at Hennepin County Medical Center and Dr. Kathleen Stringer at the University of Michigan. Michigan and UMMC are inventors on the patent.
Sepsis is a body-wide response to infection that can cause fever, low blood pressure and organ failure. Jones says it is a difficult condition to treat because it can vary from person to person. This makes sepsis a strong candidate for precision medicine approaches.
“Precision medicine is the idea of tailoring treatments to an individual’s physiology,” Jones said. “Sepsis continues to be a vexing problem, so our hope is that this serves as a springboard for developing individualized approaches instead of the shotgun approach we use now to treatment sepsis.”
He plans to conduct additional trials to validate the findings and perhaps develop enhanced diagnostics and treatments for sepsis.
“Currently, it’s labor intensive to measure these markers, but there may be ways to develop bedside assays that are quick,” Jones said.
Jones is a first-time inventor, and said that UMMC’s Intellectual Property and Commercialization Office, formerly known as the Office of Innovation Development and Licensing, was a valuable resource for him.
“They were extremely helpful with the technical aspects and navigating the patent application process,” Jones said.
And Beyond

When rural emergency departments were on the verge of closing, UMMC came up with a way to keep them open.
“We had an idea for a system where we could provide consultation to these small emergency rooms,” said Dr. Richard Summers, associate vice chancellor for research and professor of emergency medicine. “So we developed TelEmergency, where 18 emergency rooms in our state could be served by one physician who could advise on these high-acuity events.”
That was in 2003, and Summers said that in the years since, other institutions have visited the Medical Center to learn how to implement it in their own regions.
This year, the Medical Center received allowed trademarks on the names TelEmergency and TeleER. It formed the early basis for the Center for Telehealth.
“The concept of TelEmergency started at UMMC, and we realized that we had intellectual property that hadn’t been registered,” said Summers. “It codifies UMMC as the founder and of TelEmergency that through a trademark.
“We wouldn’t have been able to [get the trademark] without the help of the IPAC,” Summers said. “I had no clue where to start, but Jim Petell did and moved us through the process.”
Dr. Jim Petell, director of the IPAC, says that UMMC inventors have submitted 37 invention disclosures representing four schools and 21 departments since January 2018.
“Together with the 19 U.S. patent applications and four trademarks filed by inventors during this period, the increase in intellectual property metrics compared to previous years is impressive and demonstrates a vibrant, inventive culture at UMMC,” Petell said. UMMC is seeking to commercialize its proprietary medical innovations to benefit the institution and the people of Mississippi.
The IPAC is preparing to recognize inventors at UMMC’s first Intellectual Property ceremony on November 19. In previous years, patent recipients were recognized at the annual Excellence in Research Awards, but the increase in productivity has given the Medical Center reason to celebrate.
“What the IPAC has been able to accomplish in the last couple of years is amazing,” Summers said.


