Omicron surge creates unprecedented staff shortages as hospitalizations rise

Editor’s note: This article was updated Jan. 18, 2022, to reflect updated COVID-19 numbers.
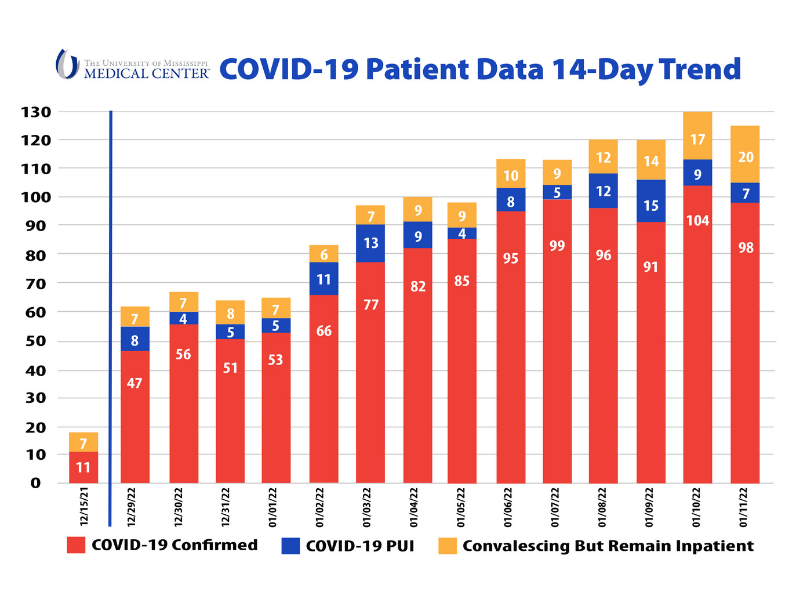
The impact of rising numbers of hospitalized COVID-19 patients at the University of Mississippi Medical Center will likely worsen before it gets better, hopefully with a downward trend to the current spike of the Omicron variant by late January or early February.
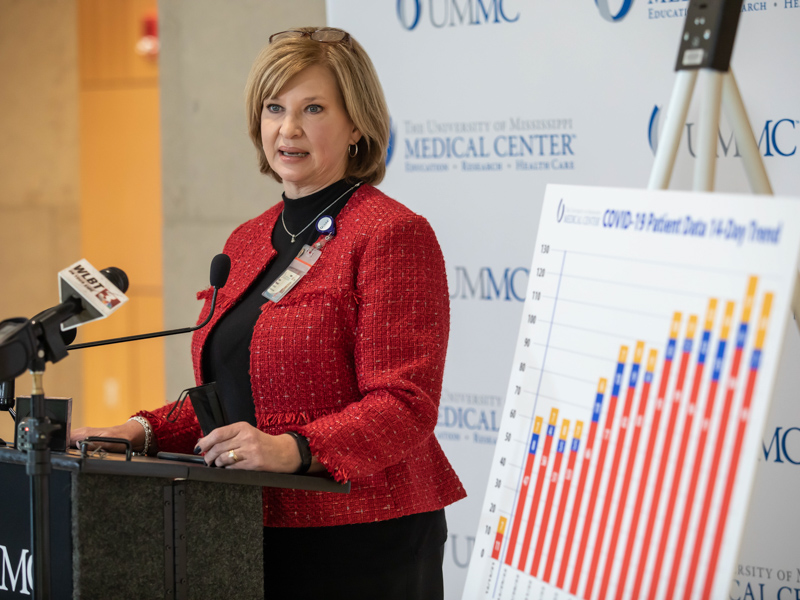
“It’s just stunning,” Dr. LouAnn Woodward, vice chancellor for health affairs and dean of the School of Medicine, told members of the media Tuesday. “We’re back to the party that no one wanted to come to.”
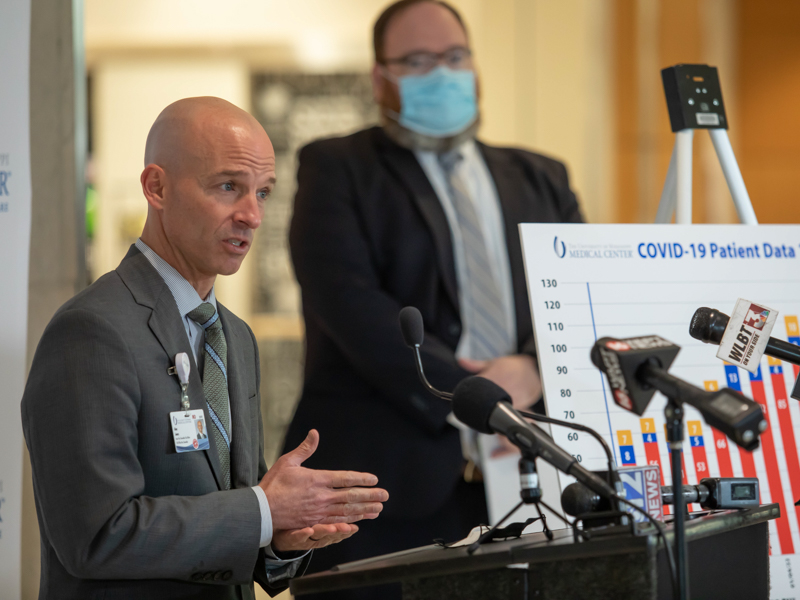
“We’re dealing with a shifting enemy, and it’s changed the rules of the game,” said Dr. Alan Jones, vice chancellor for clinical affairs and the Medical Center’s clinical COVID-19 response leader. “The sheer volume of patients is what’s overwhelming.”
As of 8 a.m. Jan. 18, the Medical Center had 130 patients who were confirmed with the virus, awaiting test results or convalescing with COVID. A breakdown: 74 adults and 19 children confirmed, and of those numbers, 24 adults and five children are in the ICU; 29 adults and two children convalescing, meaning they’re no longer infectious, but not well enough to go home; and four adults and two children awaiting test results.
Two weeks earlier, on Jan. 4, the number of patients hospitalized with COVID-19 was 100.
The morning of Jan. 18, the hospital was holding 23 admitted patients in its Emergency Department, waiting for a bed. “When the ICU gets full, when the med-surg beds get full, the ultimate place patients back up is in the Emergency Department,” said Jones, who with Woodward is an emergency medicine physician.
There are bright spots, Woodward and Jones said, but there are challenges that threaten UMMC’s mission to treat as many patients as possible:
- The Omicron virus is much more contagious than the Delta variant, but tends to result in lower ICU numbers. But if you’re sick enough for ICU care, “it’s just as bad as Delta,” Woodward said.
- Before the pandemic, the Medical Center’s average number of nurse openings was about 70. “We would shudder at that,” Jones said. Today, that number is 360, fueled mainly by nurses leaving the profession or lured away during a competitive market.

Adding to that is higher numbers of employees who are at home recovering from the virus or under quarantine. “It’s been 175 a day at some points,” Jones said of the 10,000 employee Medical Center. Of that number, today there are 80 to 90 front-line caregivers out on isolation alone.
“This is happening across the country,” said Woodward, UMMC’s COVID-19 incident commander. “Fifty-five to 59 beds are closed because we don’t have the staff to staff them.”
Although the Department of the Defense and the nonprofit Samaritan’s Purse in late summer set up and staffed COVID-19 treatment tents in UMMC parking lots. “We don’t see the cavalry coming over the horizon,” Jones said. If that was even an option, it would take weeks – and by that time, Mississippi might be on the other side of the current surge.
- During the Delta surge, between five and 10 people a day came to the Emergency Department with COVID-19 symptoms. “We’re triple that number now,” Jones said.

And although the Medical Center would never discourage anyone from getting emergency care if they believe they need it, Jones said, he encourages a trip to the ED for symptoms that are out of the ordinary- for example, chest pain, difficulty breathing or fever that won’t go down.
“I would not use the ED as a (COVID-19) testing station. We are overwhelmed,” Woodward said.
- Some patients are so ill they would benefit from monoclonal antibodies, and the only one effective against Omicron is in very short supply statewide, he said. UMMC uses all of the allotment it receives from the Mississippi State Department of Health. “We have tried to focus on the patients at the very highest risk, including the unvaccinated,” Jones said.
Jones said UMMC is accepting patients every day as the state’s top trauma center and with the state’s only children’s hospital. But, it must consider multiple factors when accepting the transfer of patients from other hospitals, whether sickened from COVID-19 or something else.
“There are certain types of patients that only UMMC can take ... but we must look at how we can best deploy our resources,” Jones said. “But when the system bogs down, hospitals are fighting with both arms behind their back.”
Mississippi MED-COM, housed at UMMC within the Mississippi Center for Emergency Services, provides emergency communications for hospitals and emergency providers throughout the state. Its staff tracks available ICU and regular patient beds statewide, on a minute-to-minute basis, and evaluates patient transfer requests based on what level of care the patient needs and the availability of resources.

On Tuesday, the Mississippi State Department of Health activated the mandatory Mississippi COVID System of Care to allow the most critically ill patients to be transferred for care without overburdening any one hospital. It means that when no beds are available, MED-COM must direct patients to hospitals on a rotating basis based on geography and resource availability.
“There are a lot of variables,” said Dr. Jonathan Wilson, chief administrative officer and COVID-19 incident manager. “We are trying to get patients to the best level of care possible.”
Where do the Medical Center and the state’s hospitals go from here?
“We are navigating this the best we can, but it’s a day-to-day, hour-to-hour process,” Jones said. “We’re doing the best we can to spread (our) resources around.”
The trajectory of Omicron cases now looks like a pattern of a rapid rise, then a rapid fall, Woodward said. But for now, “the only thing that will really help is to flatten the curve of people who are hospitalized.”


