Vitals for Nursing: April 25, 2023
Prescription Prior Authorization is the process by which providers verify a payer's willingness to cover a medication for a specific patient. Before approving a treatment for coverage, payers may need to review information about the patient. For example, the payer may ask questions about associated diagnoses and previous treatments.
Prior Authorization inbasket messages will route to a department or clinic support pool for ambulatory and to the meds authorizing provider for inpatient. The top level of the PA Inbasket folder includes patient names, medications, and a “Request Status” column. Clicking on individual messages will reveal more details. These messages can be removed from Inbasket either by resolving the PA request or by forwarding the message with responsibility to another staff member.
(Review attached Tip Sheet located on the Epic Resource Center for additional information Prescription Prior Authorization Tip Sheet)
Prior Authorization Request Status Types:
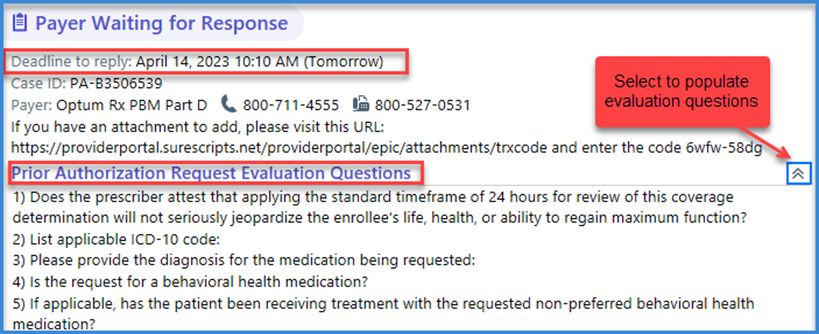
1. Payer Waiting for Response: (PA requests evaluation sets to be answered)
- Some PAs request completion of evaluation question sets which route to Inbasket. These requests need to be answered prior to the deadline to reply to continue processing the request.
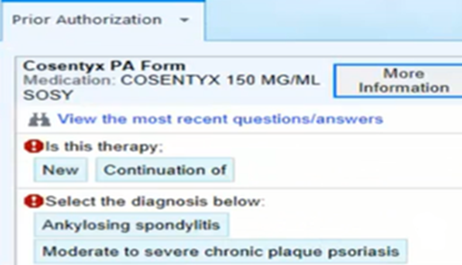
- Select a Plan- Select a plan to find the correct form. Once chosen, additional questions will need to be completed.
2. Closed: (Review note from payer)
- Plan not enabled for EPA. - PBM may support EPA but patients plan is not connected to EPA. Submit PA by another method. – (Covermymeds or manually)
- Request cannot be processed for the member plan submitted. – PBM may support EPA but patients plan is not connected to EPA. Submit PA by another method.
- EPA not supported - Submit PA by another method.
- Cannot match drug for the NDC sent - Ordering provider should review medication and prescribe appropriate drug.
- PA not required for patient/medication - Medication does not require PA. No further action.
- Closed - Other- Not able to process request through EPA. Submit PA by another method.

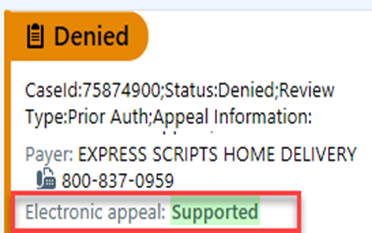
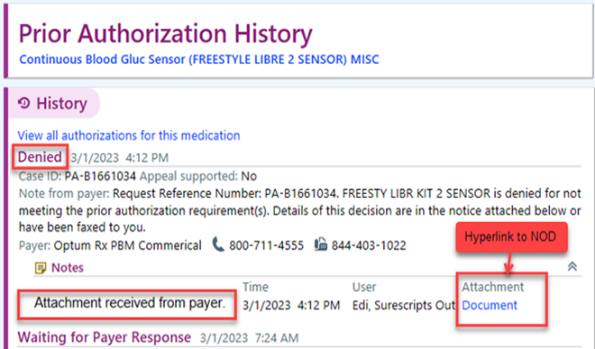
4. Denied:
- Review PA note - There may be an option to submit an electronic appeal if supported.
Not meeting the PA requirements - The PA history will give an embedded ‘DOCUMENT’ hyperlink that will contain the Notice of denial document.
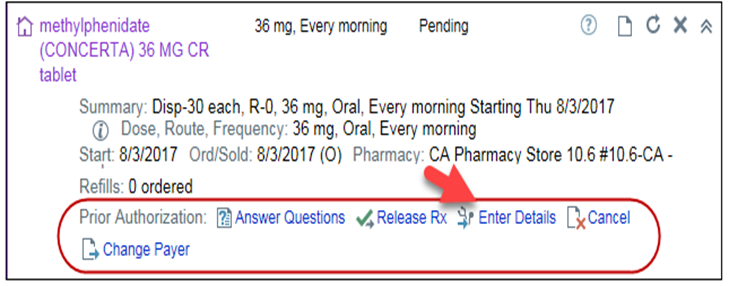
4. Waiting for Auth Details:
- Inbasket message with a question set or a URL to complete the PA. Once the user completes the e-form or fills out the form from the URL and sends to the payer, then we should receive a response from the payer in the form of a fax. The details from the fax can then be entered by clicking the link that says Enter Details from the med management order details or from the Inbasket message.
5. Canceled-Other:
- Case has already been resolved. Request already processed/final determination has been made.



