- Cancer Institute
- Cancer Research
- Cancer Registries
- Mississippi Cancer Registry
- Data and Statistics
- Lifestyle-Related Cancers
Lifestyle-Related Cancers
- Cancer Center and Research Institute
-
Cancer Research
- Cancer Research Overview
-
Cancer Registries
- Cancer Registries Home
- UMMC Cancer Registry
- Mississippi Cancer Registry
- Clinical Trials
- Programs
- For Students and Trainees
- Patient Support
- Give Now
- In the News
- Contact Cancer Center and Research Institute
- CCRI Leadership
HPV-related Cancers in Mississippi, 2003-2021
The Human Papilloma Virus (HPV) increases the risk of certain types of cancer. A vaccine is available that can prevent the most common cancer-causing types of HPV. Unfortunately, data from the 2021 National Immunization Survey-Teen reported by the National Cancer Institute’s State Cancer Profiles shows that only 32.7% of Mississippi teens between ages 13 and 17 have received two or more doses of the HPV vaccination. Mississippi has the lowest rate of vaccination in the U.S.1 Cancers associated with HPV infections include squamous cell carcinoma of the oropharynx, rectum, anus, vagina, vulva and penis, as well as carcinoma of the cervix. Below are graphs of the trends in HPV-related cancers over the period 2003 to 2021 by race and sex, where the counts allow for such breakdown with a description of the trends occurring in each group both for the full time period and for the most recent period between 2017 and 2021. All analysis was done using SEER*Stat software2.
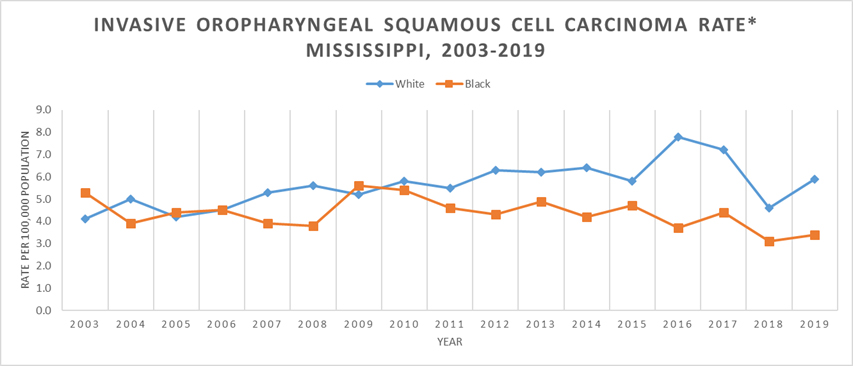
Approximately 70% of squamous cell carcinomas of the oropharyngeal cancers are likely associated with HPV.3 Additionally, cancers of the oral cavity and pharynx including the oropharynx can be associated with other modifiable risk factors, tobacco and alcohol use. The rate of oropharyngeal squamous cell carcinoma cannot be broken down by both race and sex due to how rare this cancer is particularly in black females. Over the period from 2003 to 2021, the white population had significantly higher rates of oropharyngeal squamous cell carcinoma than the black population in 2008, 2012, 2014, 2016 and 2017-2021. Between 2003 and 2016, the white population experienced a significant increase of 3.60% annually. Then, between 2016 and 2021, the white population experienced an observed decrease of 5.08% annually. These patterns translate into an observed average annual percent increase of 1.1% over the full time period of 2003-2021 for the white population. Between 2003 and 2013, the black population experienced an observed increase of 0.75% annually. Then, between 2013 and 2021, the black population experienced a significant decrease of 5.63% annually. These patterns translate into an observed average annual decrease of 2.1%. The graph clearly demonstrates the widening of the gap between the rates of the white and black populations beginning in 2011. For the latest five-year time period between 2017 and 2021, the trend for the white population was a decrease of 4.06% annually. The rate for the black population during this period decreased at a rate of 8.49% annually. The changes for both groups between 2017 and 2021 were not statistically significant.
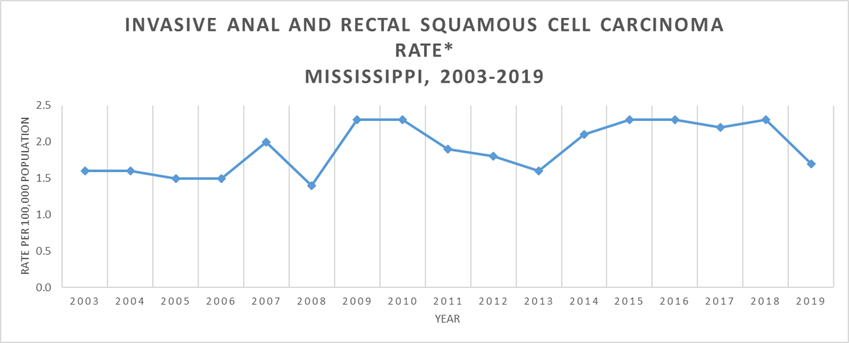
Approximately 91% of the squamous cell carcinomas of the anus and rectum are associated with HPV infection.4 Cancers of the rectum can also be associated with other modifiable risk factors, tobacco use, alcohol use and obesity. Squamous cell carcinoma of the anus and rectum are rare cancers. Thus, the data can only be presented for Mississippi as a whole and not broken down by race and sex. Between 2003 and 2021, the rates for squamous cell carcinoma of the rectum and anus increased significantly at a rate of 1.62% annually. The greatest increases were seen in both white and black females. For the latest five-year time period between 2017 and 2021, anal and rectal squamous cell carcinoma was observed to be decreasing at a rate of 2.55% annually, though this change was not statistically significant.
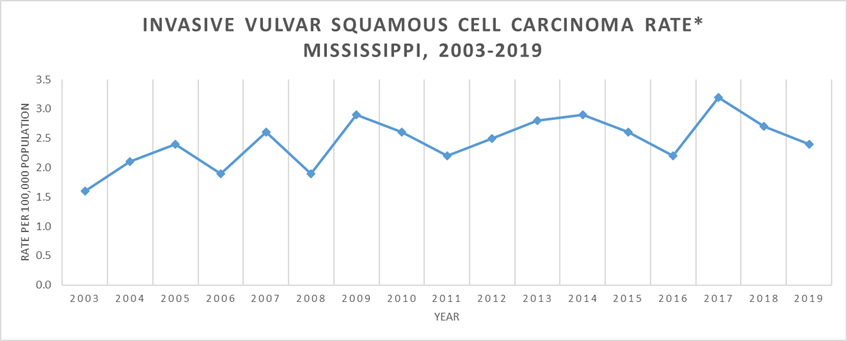
Approximately 69% of squamous cell carcinomas of the vulva are associated with HPV infection.3 quamous cell carcinoma of the vulva is a rare cancer. herefore, the rates cannot be broken out by race. or the time period between 2003 and 2021, the rates of squamous cell carcinoma of the vulva increased at a rate of 1.04% annually, though this change is not statistically significant. n the most recent five-year time period between 2017 and 2021, the squamous cell carcinoma of the vulva decreased at a rate of 9.33% annually, though this decrease was not statistically significant due to the small number of cases.
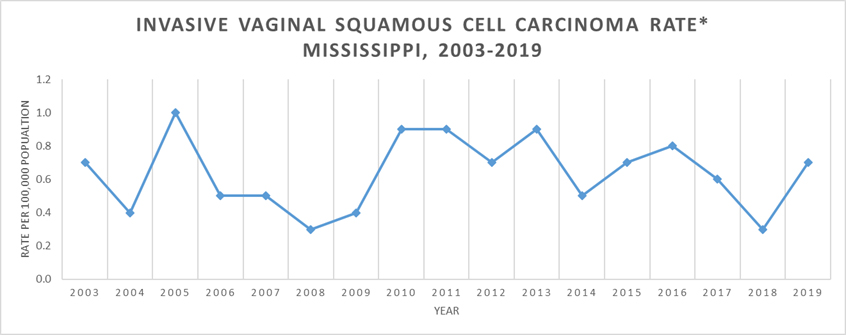
pproximately 75% of the squamous cell carcinomas of the vagina are associated with an HPV infection.3 quamous cell carcinoma of the vagina is also a rare cancer. herefore, the rates cannot be broken out by race. or the time period between 2003 and 2021, the rates of squamous cell carcinoma of the vagina remained relatively stable with only a 0.24% decrease annually. owever, for the latest five-year time period between 2017 and 2021, the rate of squamous cell carcinoma of the vagina rose 2.88% annually. his change was not statistically significant.
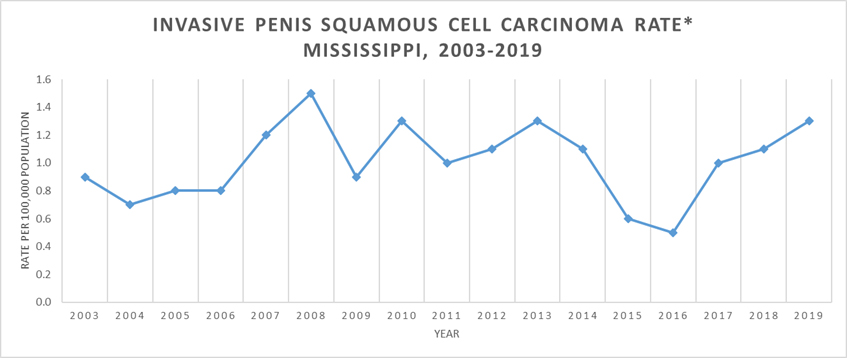
pproximately 63% of squamous cell carcinomas of the penis are associated with HPV infection.3 ike most of the other HPV-related cancers, squamous cell carcinoma of the penis is a rare cancer. herefore, the rates cannot be broken out by race. or the time period between 2003 and 2021, the rates of squamous cell carcinoma of the penis increased 1.19% annually though this increase was not significant due to the small number of cases. or the latest five-year time period between 2017 and 2021, the rate of squamous cell carcinoma of the penis increased 4.11% annually. his change was not statistically significant.
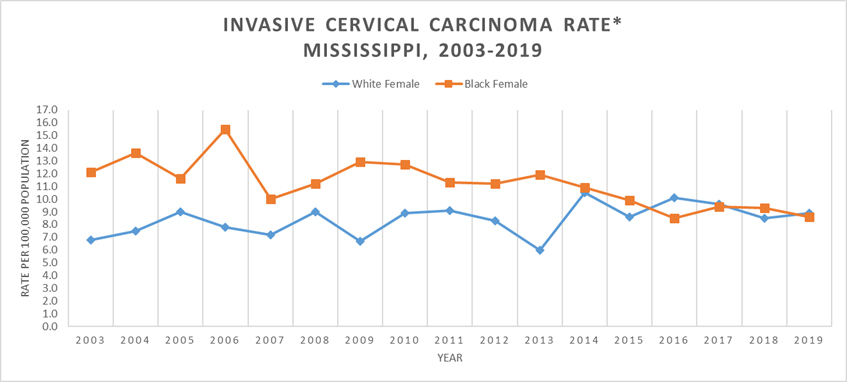
pproximately 91% of cervical carcinomas are associated with an HPV infection.3 ancers of the cervix uteri can also be associated with another modifiable risk factor, tobacco use. he rates of cervical carcinoma were higher for black females than white females between 2003 and 2015, but this difference was only statistically significant for 2003, 2004, 2006, 2009, 2010 and 2013. ver the time period from 2003 to 2021, the rate for black females dropped significantly at a rate of 2.17% annually. he rate for white females increased at a rate of 1.30% annually. his increase was not statistically significant. ver the latest five-year period of 2017 to 2021, the rate for white females slightly decreased 0.10% annually, though this change was not statistically significant. he rate for black females increased 1.15% annually, though the change was not statistically significant. he falling rate for black females coupled with the observed increasing rate for white females closed the disparity between the two groups.
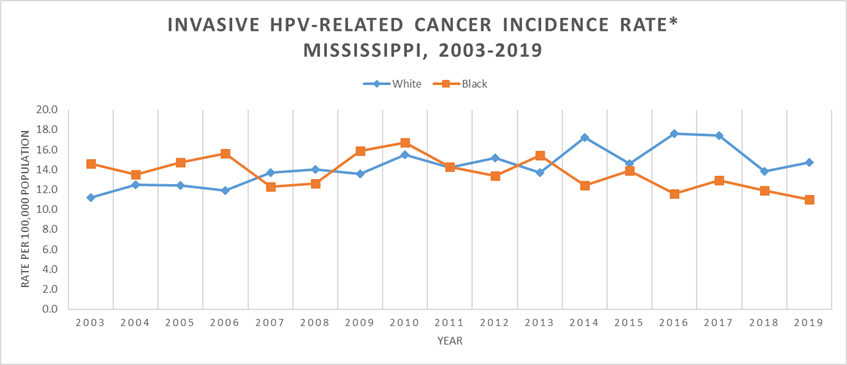
he rates of all HPV-related cancers are primarily driven by oropharyngeal carcinoma and cervical carcinoma. uring the period from 2003 to 2021, the rate for white males and white females significantly increased. hite males experienced an annual increase of 1.85% and white females experienced an increase of 1.88% annually. onversely, the rates for both black males and black females decreased, though the change was only statistically significant for black females. lack males experienced a decrease of 1.11% annually and black females experienced a significant decrease 1.45%.
or the most recent five-year time period from 2017-2021, the rates for all groups except white males decreased, though not significantly. he rate for white females decreased 1.21% annually and the rate for black females decreased 2.27% annually. or black males, the rate decreased 6.08% annually. or white males, the rate increased slightly at a rate of 0.27%.
Definitions
Age Adjusting: statistical method that allows comparisons of populations that take into account age-distribution differences between the populations. he 2000 U.S. standard population is used and applied to all of the time periods being considered. his assures that the rates do not reflect differences in the age distribution of the population.
Annual Percent Change (APC): he average annual percent change over several years. t is used to measure the change in rates over time. alculating the APC involves fitting a straight line to the natural logarithm of the data when it is displayed by calendar year.
Statistical Significance: his is a mathematical measure of the difference between groups. difference is said to be statistically significant if it is greater than what might be expected to happen by chance alone 95% of the time. ate ratios were used to assess the statistical significance between groups.
itations
1The National Immunization Survey - Teen, Hyattsville, MD: Centers for Disease Control and Prevention. reated by statecancerprofiles.cancer.gov on 06/03/2024 1:05 pm.
2Surveillance Research Program, National Cancer Institute SEER*Stat software (seer.cancer.gov/seerstat) version 8.4.3.
3Division of Cancer Prevention and Control, Centers for Disease Control and Prevention. ancer Linked with HPV Each Year [online]. 2023. [accessed May 17, 2024]. URL: https://www.cdc.gov/cancer/hpv/cases.html?CDC_AAref_Val=https://www.cdc.gov/cancer/hpv/statistics/cases.htm
Source of Data: EER*Stat Database: MS0221. Created on 4/2/2024. Mississippi Cancer Registry 2023 Submission (2002-2021) to Centers for Disease Control and Prevention, National Program of Cancer Registries.
Acknowledgement
We acknowledge the Centers for Disease Control and Prevention for their financial support under a cooperative agreement awarded to the Mississippi Cancer Registry.


