Fall 2019
- The Pulse - UMMC Anesthesiology - Archive
- Fall 2025
- Spring 2025
- Winter 2025
- Spring 2024
- Winter 2024
- Fall 2023
- Spring 2023
- Winter 2023
- Fall 2022
- Spring 2022
- Winter 2022
- Fall 2021
- Spring 2021
- Winter 2021
- Fall 2020
- Spring 2020
- Winter 2020
- Fall 2019
- Spring 2019
- Winter 2019
- Fall 2018
- Spring 2018
- Fall 2017
- Winter 2017
- Winter 2026
Anesthesia Trainees Reinforce Learning with Simulation Training
By Sara B. Robertson, M.D.
UMMC’s simulation training center, also known as the Simulation and Interprofessional Education Center (SIEC), is housed in the new school of medicine built in 2017. It is part of
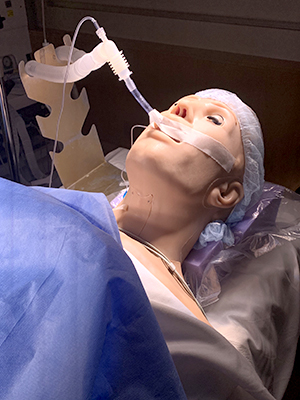
UMMC’s Office of Interprofessional Simulation, Training, Assessment, Research and Safety (ISTARS) which is provisionally accredited by the Society for Simulation in Healthcare. Even though the department of anesthesiology has long been taking advantage of the benefits of simulation for our trainees in the simulation center in the classroom wing on campus, this new facility has much more room and is updated with state-of-the-art simulation equipment.
The Office of ISTARS was awarded Provisional Accreditation from the Society for Simulation in Healthcare (SSH) in December 2018. This provisional status will be in effect from December 1, 2018, through December 31, 2020, during which time preparations for application for full accreditation will be undertaken. Provisional accreditation recognizes the UMMC ISTARS facility as a member of the foremost international simulation society and a leader in use of best simulation education practices.
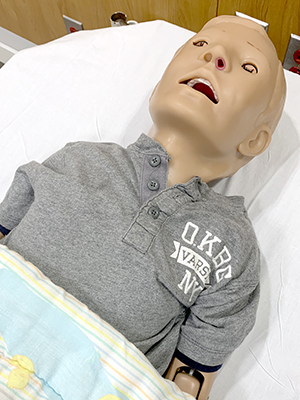
Simulation encompasses use of artificial models (computer models, skills trainers, and manikins) with varying degrees of fidelity to the human state, application of role-playing to model communication among professional team members and with patients and family, and interaction of trainees with standardized patients in scenarios mimicking actual clinical encounters. This training environment permits trainees to develop proficiency in life-saving, invasive, communication and clinical reasoning skills. Simulation also can dynamically assess critical needs in patient care processes, unit organization and team relationships within actual practice structures, all of which advance patient safety and reduce medical errors. Below are some of the skills related to anesthesia training taught at the SIEC:
Basic airway management
Airway anatomy and evaluation
- Mask ventilation
- Oropharyngeal and nasal airways
- Direct laryngoscopy and intubation
- LMA placement
Difficult airway management
Difficult airway algorithm
- Airway anesthesia
- Fiber-optic intubation
- Intubation with Fastrach and CTrach LMA
- Cricothyrotomy and jet ventilation
- Intubation over bougie
- Retrograde wire intubation
Spinal access
- Anatomy of the spine and thecal spaces
- Sterile procedure performance
- Lumbar puncture kit contents
- Lumbar puncture
Peripheral vascular access
- Venipuncture
- Peripheral IV catheter placement
- Arterial catheterization kits
- Arterial catheter (radial and femoral) placement
Central venous catheterization
- Anatomy of central veins
- Sterile procedure performance
- Triple lumen catheter kit contents
- Internal jugular vein catheter placement
- Subclavian vein catheter placement
- Femoral vein catheter placement
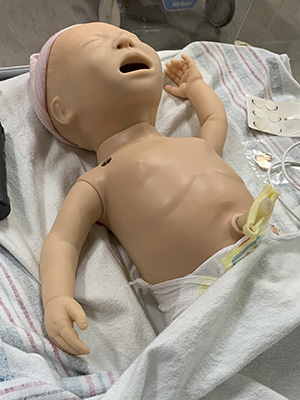
Our anesthesia residents and fellows participate in six to eight crisis risk management (CRM) simulation sessions yearly. Scenarios include pulmonary embolism, Wolfe-Parkinson-White syndrome, Advanced Cardiac Life Support (ACLS), laryngospasm, neonatal resuscitation, and many more. Each resident also is required to participate in the Pig Trachea Workshop, retrograde intubation workshop, and the one-lung ventilation and lung isolation workshop. Dr. Henrique Vale is the course director for all the simulation sessions for the residents. Drs. Lakshmi Kurnatala, Ken Oswalt and Tan Graham have also spearheaded a regional anesthesia workshop for the department.
By attending these simulation sessions and workshops, our trainees are better able to care for our patients by gaining insight and knowledge surrounding sometimes less commonly encountered clinical scenarios and by getting real-time feedback on their performance. We hope to be able to add more simulation sessions and workshops for our faculty and staff as well in the future.


