NOVEL CORONAVIRUS UPDATES | COVID-19
In an effort to protect everyone that enters any of our hospitals, we are announcing some temporary restrictions to our hospital visitor policy that may affect who can accompany you during an upcoming appointment or scheduled procedure. These changes also affect hospital-based clinics and procedure areas.
Beginning Monday, March 16 at noon, if you are visiting any of the UMMC Jackson-based hospitals (University, Wiser, Batson and Conerly) then the following restrictions will apply:
- Adult patients are not permitted to have visitors except in certain circumstances listed in the new policy.
- Pediatric patients (Children’s of Mississippi) are permitted to have only two adult visitors, but both must be parents, guardians or caregivers.
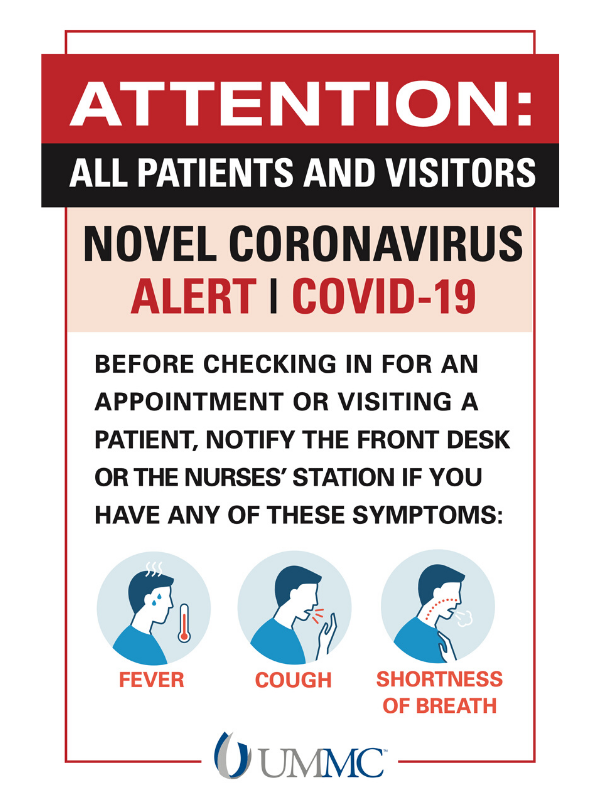
All patients and visitors needing to enter a hospital facility, including for an appointment at a hospital-based clinic or procedural unit, will enter through one of two available entrances:
- The front entrance of University Hospital (under the overhang facing State Street near Garage A)
- The side entrance to Wiser Hospital for Women and Children (under the overhang facing Garage B)
All patients and visitors will be screened at the two entrances listed above. Patients who exhibit symptoms associated with respiratory illness (fever, runny nose, cough, shortness of breath) or report they have recently visited an area identified as a location experiencing a COVID-19 outbreak will receive further evaluation to determine next steps. Visitors that meet any of that criteria will not be allowed to enter under any circumstances.
Similar changes at UMMC Grenada and UMMC Holmes County went into effect earlier today.
To view the policy for Jackson-based hospitals, click here. To view the policy for UMMC Grenada and Holmes County, click here.
While we understand some of these changes may cause you and your family and friends discomfort, the safety of our patients, visitors, employees and students is our top priority.
We appreciate your understanding as we try to take very step possible to reduce the spread of COVID-19.
Updated Coronavirus, COVID-19 Information

Last updated Sunday, March 16, at 10:45 a.m.
This page will be frequently updated to reflect current information related to the coronavirus and COVID-19.
The University of Mississippi Medical Center continues to closely monitor COVID-19 cases throughout the state, nation and world.
On March 11, the Mississippi State Department of Health (MSDH) reported the state’s first positive case of COVID-19, a Forrest County man who recently traveled to Florida. The patient voluntarily isolated himself at home to prevent further transmission to others and wasn’t hospitalized.
Nine more cases have since been identified, among them a Forrest County woman over 65 who recently traveled to North Carolina and was hospitalized; a Forrest County man who recently traveled to Florida, and who is home self-isolating and didn’t require hospitalization; a Leflore County woman who is home self-isolating and didn’t require hospitalization; a Pearl River woman over 65 who was hospitalized; and a Copiah County woman over 65 who was hospitalized.
MSDH reported the most recent four cases on March 15. Two of those cases are in Hinds County and one each are in Copiah and Pearl River counties. That brings total cases to two in Hinds County, two each in Copiah and Pearl River counties, one in Leflore County and three in Forrest County.
The Hinds County cases are two students, one at Jackson State University and one at UMMC. Both are self-isolating at home, and the UMMC student did not return to campus after the student’s diagnosis during spring break.
MSDH is investigating all cases to limit spread of the virus.
COVID-19, which originated in Wuhan City in China’s Hubei Province, has caused 5,833 deaths worldwide as of noon March 15. The vast majority – 3,085 – were in mainland China, statistics from the Center for Disease Control and Prevention show. Fifty-seven deaths have occurred in the United States, five in California, three in Florida, two in New York, one in Colorado, one in Georgia, one in Kansas, one in Louisiana, one in New Jersey, one in South Dakota, one in Virginia and 40 in Washington state. It has infected 156,400 people globally, 2,952 of those in the United States and 80,995 in mainland China. The World Health Organization on March 11 declared COVID-19 a global pandemic.
Most acute care hospitals in Mississippi have the facilities necessary to screen, isolate and care for COVID-19 patients. The Medical Center currently is not caring for any COVID-19 patients. If this changes, we have a highly skilled medical team trained to respond.
UMMC has taken action in recent weeks to protect patients, their families and employees that includes:
- Working hand in hand with the Mississippi State Department of Health (MSDH) and the Centers for Disease Control and Prevention (CDC), we have processes in place to identify who should be screened for COVID-19, as well as answer questions from the public. If testing is needed, patient samples will be forwarded to MSDH.
- A Medical Center leadership team is spearheading preparations and response, and UMMC’s approximately 10,000 employees are being educated on COVID-19 protocol, measures they should take if they have contact with a potential COVID-19 patient, and steps they and the public can take to avoid infection.
- We are asking all patients who come to our clinics and hospitals about their travel history and possible or confirmed contact with someone with a laboratory confirmed COVID-19 diagnosis, and we are directing patients at all clinic locations to use a facemask if they have a fever and cough.
The influenza season remains very active in Mississippi, and Medical Center infectious diseases specialists say that’s the immediate threat to residents. They urge anyone who has not been immunized against the flu to do so, and emphasize that it’s not too late in the season to get the vaccine.
Click here for COVID-19 Clinical Resources for Mississippi Health Care Professionals
Answers to frequently asked questions about coronavirus globally and in Mississippi:
The questions will be frequently updated to reflect current information related to the coronavirus and COVID-19.
(Sources: UMMC Division of Infectious Diseases; UMMC Infection Prevention: U.S. Centers for Disease Control and Prevention; World Health Organization)
Q: If I live in Mississippi, am I at risk for getting COVID-19?
A: The University of Mississippi Medical Center continues to closely monitor COVID-19 cases throughout the state, nation and world.
On March 11, the Mississippi State Department of Health (MSDH) reported the state’s first positive case of COVID-19, a Forrest County man who recently traveled to Florida. The patient voluntarily isolated himself at home to prevent further transmission to others and wasn’t hospitalized.
Nine more cases have since been identified, among them a Forrest County woman over 65 who recently traveled to North Carolina and was hospitalized; a Forrest County man who recently traveled to Florida, and who is home self-isolating and didn’t require hospitalization; a Leflore County woman who is home self-isolating and didn’t require hospitalization; a Pearl River woman over 65 who was hospitalized; and a Copiah County woman over 65 who was hospitalized.
MSDH reported the most recent four cases on March 15. Two of those cases are in Hinds County and one each are in Copiah and Pearl River counties. That brings total cases to two in Hinds County, two each in Copiah and Pearl River counties, one in Leflore County and three in Forrest County.
The Hinds County cases are two students, one at Jackson State University and one at UMMC. Both are self-isolating at home, and the UMMC student did not return to campus after the student’s diagnosis during spring break.
MSDH is investigating all cases to limit spread of the virus. This is a rapidly evolving situation, and the risk assessment can change daily.
Q: Who should be screened for COVID-19?
A: As COVID-19 spreads through communities, guidelines from the U.S. Centers for Disease Control and Prevention on who should be screened are changing and may continue to change.
Screenings will take place on someone experiencing fever and signs/symptoms of lower respiratory illness (cough, shortness of breath), and, in the last 14 days before symptoms appeared, had either a history of travel from any of five geographical areas outside the United States: China, Japan, South Korea, Italy and Iran; or close contact with a laboratory-confirmed COVID-19 patient.
In addition, given the increased evidence of community spread within the United States, CDC updated its guidelines on March 4 to say a physician's suspicion for COVID-19 is sufficient indication for testing for what appears to be a milder case not requiring hospitalization. They will base this on the local outbreak situation, and evaluation of those with severe respiratory illness of unclear origin.
Q: If I believe I have symptoms of COVID-19 and believe I meet one or more of the conditions that warrant screening or testing, should I come to UMMC?
A: Most acute care hospitals in the state are prepared to receive COVID-19 patients, including screening, isolation and care as needed. Unlike in the Ebola crisis of a few years ago, COVID-19 patients do not receive added benefit from a higher level of care offered by medical centers that are tertiary, meaning those that treat more severe conditions that require specialized knowledge and more intensive health monitoring.
Q: Regardless of where I might seek care, what should I do first?
A: Call ahead to a health care provider or emergency department and tell them if you are having symptoms that might be caused by COVID-19. By calling ahead, you allow providers time to take steps to keep other people from potential exposure before your arrival. Providers will use a screening tool to determine if you need to be isolated and tested for the virus.
If you are at home, as much as you can, stay in a specific room away from other people and pets. Use a separate bathroom if you can. Stay home except to get medical care. Wear a facemask if you are around other people in a room or vehicle, around pets, or in a provider’s office.
Wash your hands frequently with soap and water for at least 20 seconds. Cover your coughs and sneezes with a tissue, throw away the tissue, then immediately wash your hands. Avoid sharing personal household items with people or pets, and clean all high-touch surfaces daily.
If your symptoms worsen, including difficulty breathing, seek prompt medical attention. If you have a medical emergency and need to call 911, tell the dispatcher that you have or are being evaluated for COVID-19. If possible, put on a facemask before help arrives.
Q: Is anyone more susceptible to COVID-19 compared with the general population?
A: Any person, of any age, can be infected with COVID-19. Those with serious health conditions such as chronic obstructive pulmonary disease, cancer or other illnesses that compromise the immune system are more likely to experience complications from COVID-19, flu or pneumonia. The very young and the very old also are often more at risk.
Q: How deadly is COVID-19?
A: We don’t fully know, but signs suggest many people have had mild cases and recovered without special treatment. The head of the World Health Organization said on Tuesday that the global mortality rate for COVID-19 was 3.4 percent, which is higher than previously estimated. It is a figure that primarily reflects the outbreak in China, where the vast majority of cases are. The figures are expected to change over time and vary from place to place, WHO says.
In comparison, the Severe Acute Respiratory Syndrome, or SARS, coronavirus outbreak of 2003 had a fatality rate of 9.6 percent. Middle East Respiratory Syndrome, or MERS, coronavirus has a 34.4 percent fatality rate, with cases still occurring since an initial outbreak in September 2012, WHO estimates. The fatality rate for the seasonal flu, based on much more complete data, is less than 1 percent.
Q: Is there an immunization or anti-viral drug for COVID-19?
A: There’s no vaccine and no drug. Patients can use over-the-counter medications to relieve symptoms, such as cough syrup or ibuprofen/acetaminophen for fever. A number of biotech and pharmaceutical firms in several countries are developing a vaccine, but even if clinical trials are successful, further testing and regulatory action would be needed before a vaccine could become available. That could take a year to 18 months, officials with the National Institute of Allergy and Infectious Diseases say.
Q: What are the main symptoms of COVID-19? Are they the same for the flu?
A: Patients with confirmed COVID-19 have mild to severe respiratory illness accompanied by fever, cough and shortness of breath, and that can be true with flu. Just as with the flu, the symptoms of COVID-19 may or may not be mild.
Q: What is the incubation period for COVID-19?
A: The length of time between exposure to the virus and developing symptoms is estimated at anywhere from two to 14 days.
Q: How does COVID-19 spread?
A: The virus is spread by droplets created by coughing or sneezing, the same way the flu is spread. Someone can inhale the droplets and be infected, or touch their eyes, nose or mouth fingers that have been exposed to droplets. Spread can also occur from touching a contaminated surface and introducing the virus to your nose or mouth. How easily a virus spreads person to person can vary, and it’s not clear how easily COVID-19 spreads from person to person.
Q: What will UMMC do if someone who might have COVID-19 comes to the Emergency Department or another outpatient area?
A: The Medical Center is questioning all patients arriving at the Emergency Department or any other outpatient areas, about their history of travel outside this country, and their exposure to any person who has traveled outside of the United States or who has a laboratory-confirmed diagnosis of COVID-19.
Screenings will take place on someone experiencing fever and signs/symptoms of lower respiratory illness, and, in the last 14 days before symptoms appeared, had either a history of travel from any of five geographical areas outside the United States: China, Japan, South Korea, Italy and Iran; or close contact with a laboratory-confirmed COVID-19 patient.
In addition, given the increased evidence of community spread within the United States, CDC updated its guidelines on March 4 to say a physician's suspicion for COVID-19 is sufficient indication for testing for what appears to be a milder case not requiring hospitalization. They will base this on the local outbreak situation, and evaluation of those with severe respiratory illness of unclear origin.
If someone screened at the Medical Center meets the criteria for possible COVID-19 exposure and is showing symptoms of the disease, they will be immediately quarantined to minimize exposure to other patients and the health care staff. Providers will put a surgical mask on them, take them to a private room and begin the process of minimizing contact and exposure to the virus by others.
Providers entering their rooms will wear personal protective gear – special masks, eye protection, gloves, gowns and other protection as necessary. No visitors will be allowed except for a child with a single parent.
Q: If you have COVID-19 but don’t have any symptoms, can you still spread it?
A: Yes – you can shed the virus and make others ill, even if you are not showing symptoms.
Q: What’s the treatment for COVID-19?
A: There is no antiviral treatment, but instead those infected should receive supportive care to relieve symptoms. This can range from over-the-counter medications to relieve symptoms at home, to hospitalization for more severe breathing issues.
Q: How can I protect myself from getting COVID-19?
A: First and foremost, wash your hands properly and often – with soap and water for at least 20 seconds. If that’s not available, use an alcohol-based hand sanitizer. Avoid touching your eyes, nose and mouth with unwashed hands; avoid close contact with people who are sick; stay home if you’re sick; cover your cough or sneeze with a tissue, then throw the tissue in the trash; and clean and disinfect frequently touched objects and surfaces.
Q: Will wearing a mask in the general public protect me from COVID-19?
A: The CDC does not recommend that people who are well wear a facemask to protect themselves from respiratory diseases such as COVID-19. The CDC does, though, recommend people wear them who show symptoms of COVID-19 to help prevent the disease’s spread to others.
Q: Should I fly now?
A: There have been no restrictions placed on flying inside the United States, although travel to some other countries, including China and South Korea, has been restricted. If you have a fever and respiratory symptoms, you shouldn’t fly if at all possible, and if you do, you should wear a mask on the plane.
But, the same principles apply on contracting COVID-19. It’s spread by respiratory droplets generally emitted from a cough or sneeze, and experts say that they can travel up to six feet. That means people sitting closest to someone with COVID-19 or another coronavirus are at highest risk of becoming infected themselves.
Airlines such as Delta use an EPA-registered disinfectant on all flights that is rated to combat many communicable diseases.
Q: Will the warmer weather stop COVID-19?
A: It’s not yet known if weather and temperature impact the spread of the virus.
Q: Should I avoid contact with my pets if I contract COVID-19?
A: The CDC recommends that you avoid contact not just with people, but with animals including pets if you have the virus. If possible, have another member of the household care for your pets while you are sick, and avoid contact with your pet such as snuggling, petting, being kissed or licked, and sharing food. If you must care for your pet, wash your hands before and after interaction and wear a facemask. There have been no reports of pets or other animals becoming sick with COVID-19, and no reports of animals in this country being a source of COVID-19 infection but the CDC still advises restricted contact if you have the virus.


