|
Bringing greater research awards, record-setting fundraising, scientific discoveries and further growth in academic endeavors to the state of Mississippi, 2016 turned out to be a remarkable year for the Medical Center. Take a moment to once again read the top stories of your successes. Without our strong leaders and dedicated employees, we would be unable to accomplish our goal of "A Healthier Mississippi." You are what made 2016 a year of achievement. The Division of Public Affairs is privileged to tell the stories of your accomplishments. We look forward to a year of even greater advances in 2017.
|
|
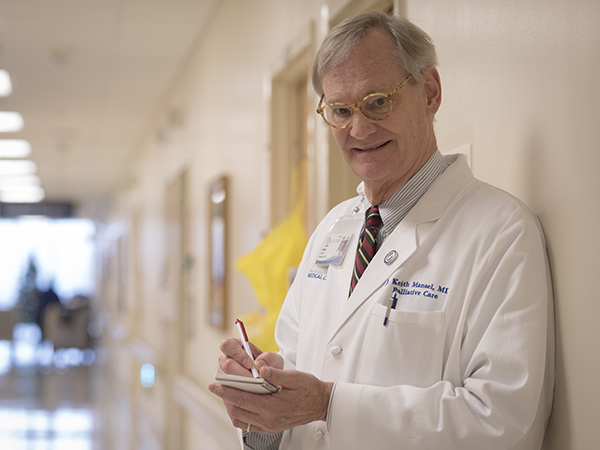
Adults facing a serious, or even life-ending, illness harbor at least two different types of hopes, said Dr. J. Keith Mansel, professor of medicine and new director of adult palliative care.
|
|
Editor's Note: This story first appeared in the Dec. 29, 2016 issue of eCV, the Medical Center's electronic newsletter. Packer was the runner-up contestant on the Big Fan program that aired on Jan. 9, 2017. John Clark Packer is a Big Fan, indeed. Closest to the UMMC Children's Miracle Network coordinator's heart are the Mississippi State Bulldogs: He traveled back and forth to Omaha, Nebraska - twice - to watch the baseball team make it to the championship game of the College World Series in 2013; he's been to several of the football team's school-record seven consecutive bowl games; and he even rented an apartment across the street from the MSU campus so he could have a place to stay after night and weekend games.
|

|

|
Several interesting events are scheduled for the upcoming weeks at the Medical Center.
|